This week we’re talking about a case as a lens for discussing Tylenol toxicity and Acute Liver Failure. These relatively common critical care presentations are essential knowledge for anyone practicing in the ICU. Listen in for some key discussion both about toxicology and the diagnosis and management of acute livery injury and failure.
Meet Our Guests
Kalaila Pais received her MD from Howard University College of Medicine and is currently a second year internal medicine resident at BIDMC. She is interested in pulmonary and critical care, as well as medical education. She also had the idea for this episode and was essential in its writing and production.
Hima Veeramachaneni received her MD from University of Missouri-Kansas City School of Medicine, and her residency at Emory where she was also a Chief Resident at Grady Memorial Hospital. She is a gastroenterologist and completed her GI and transplant hepatology training at Emory. She is also now doing a critical care medicine fellowship year.
Case Presentation
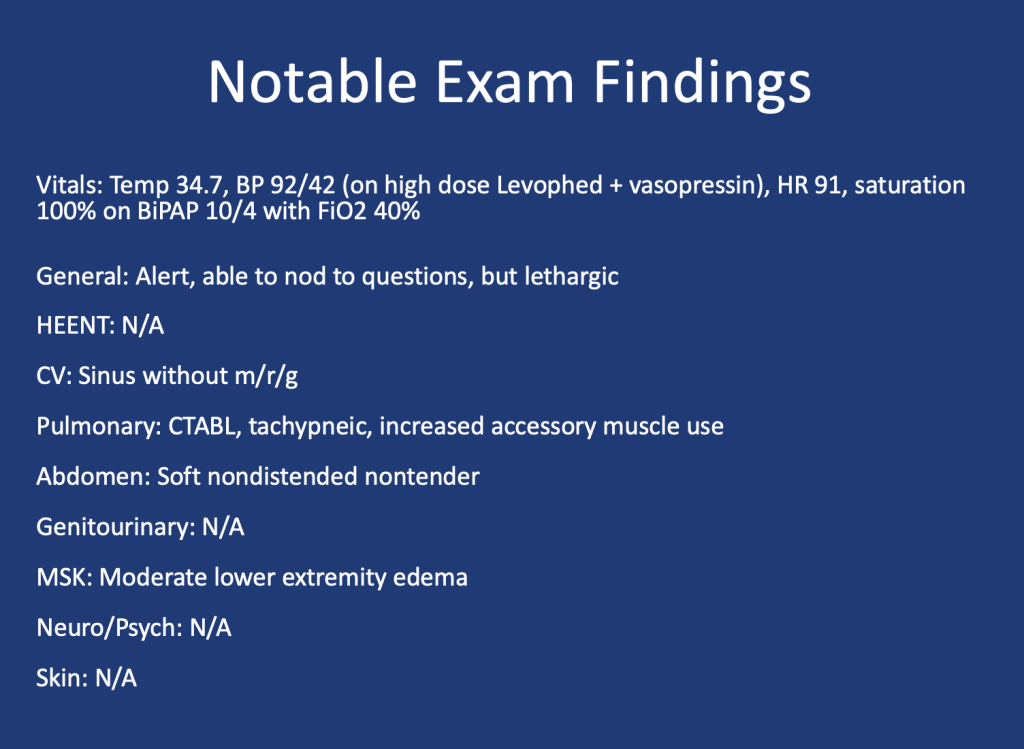
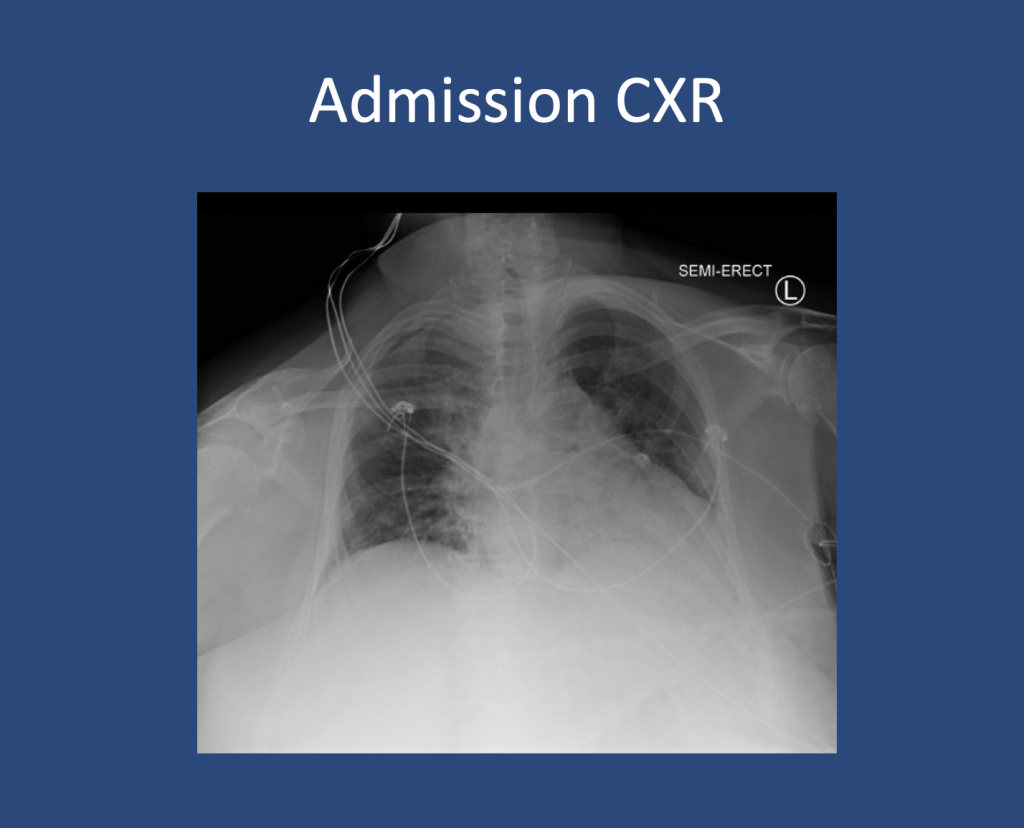
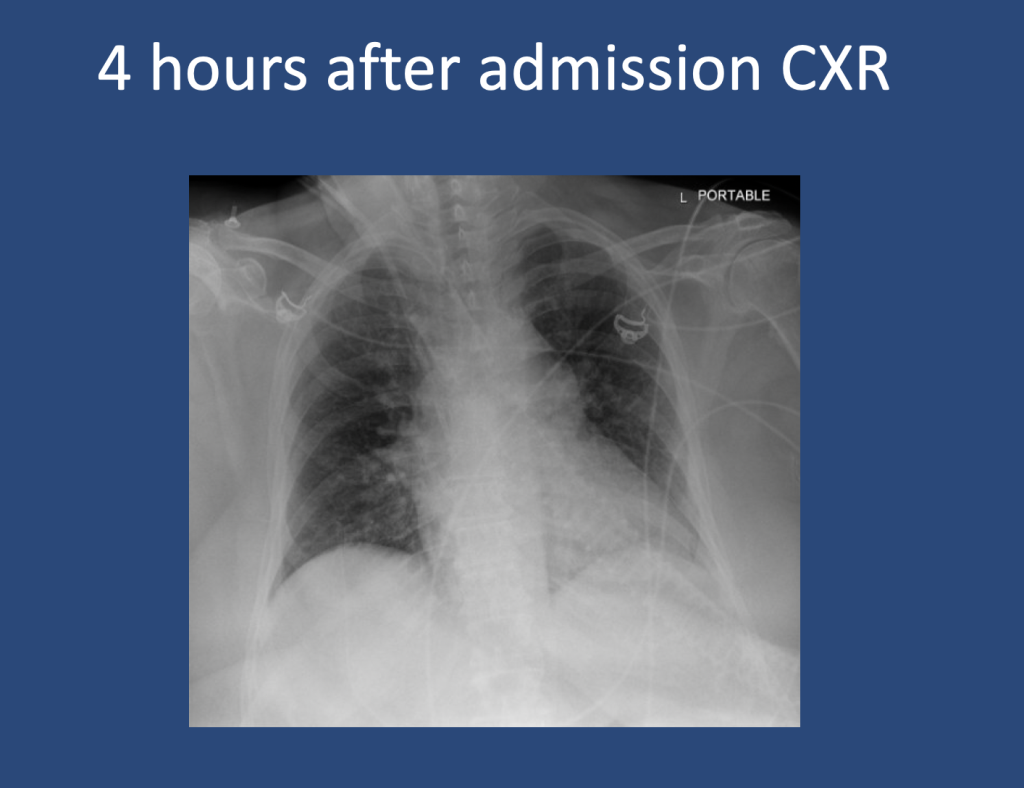
Presentation: Patient found down, surrounded by liquor bottles, with coffee-ground emesis, hemodynamic instability, scleral icterus, and metabolic derangements.
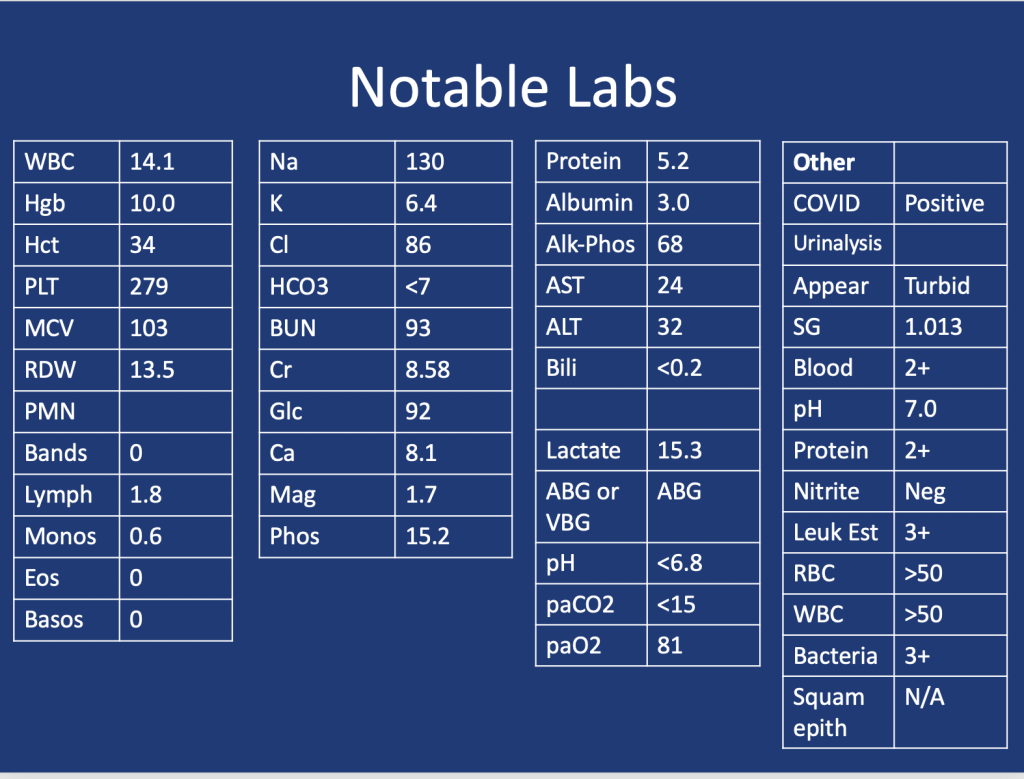
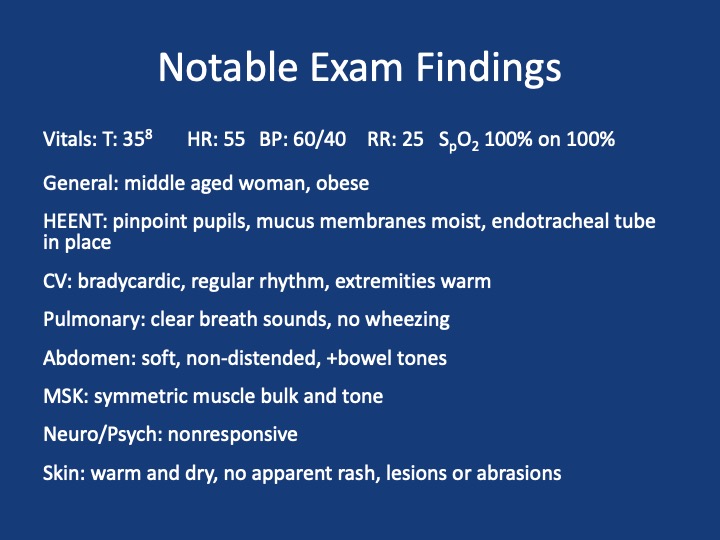
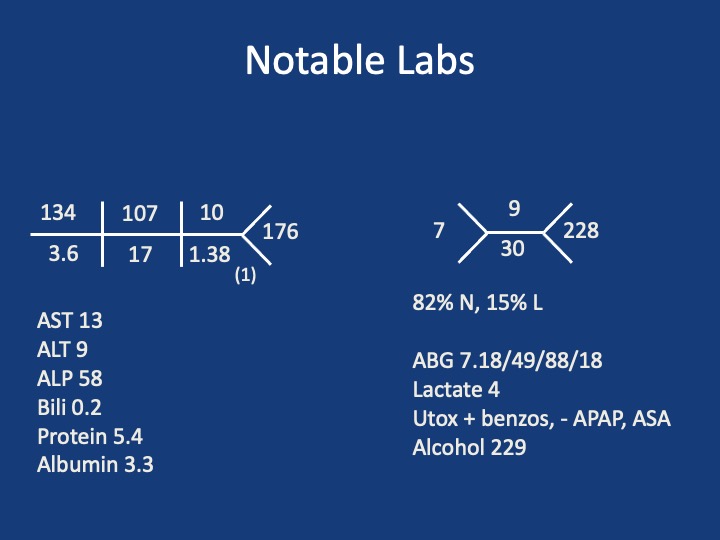
Key Lab Findings:
- Severe transaminitis (AST >10,000, ALT ~3,000).
- Elevated bilirubin (5.8), lactate (16), and INR (>2).
- Metabolic acidosis with a pH of 7.04.
- Tylenol level: 41 (slightly elevated but inconclusive without ingestion timing).
Key Learning Points
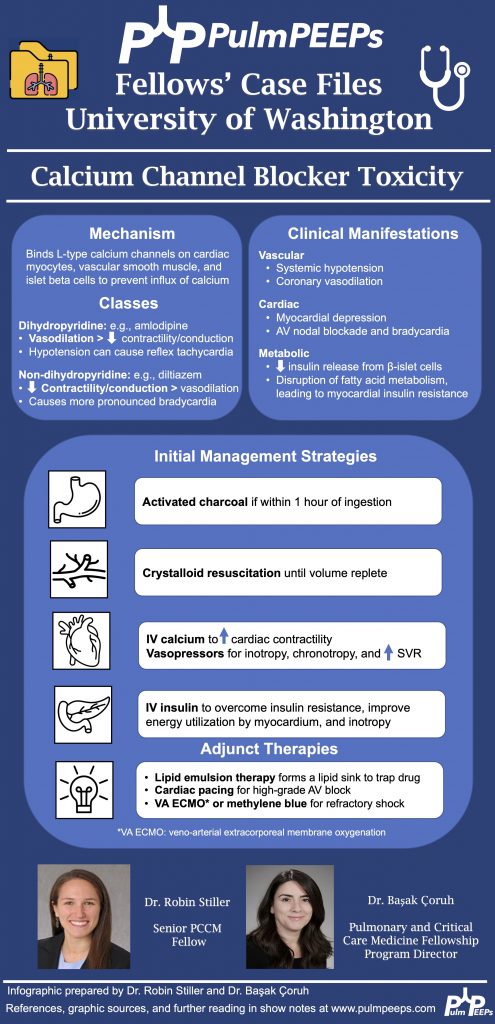
Infographic:
Acute Liver Injury vs. Acute Liver Failure
- Acute Liver Injury (ALI): Elevated liver enzymes without encephalopathy or significant synthetic dysfunction.
- Acute Liver Failure (ALF): Defined by:
- Presence of encephalopathy.
- Coagulopathy (elevated INR).
- Rapid onset (<26 weeks) in patients without pre-existing liver disease.
- ALF often leads to complications such as cerebral edema, which necessitates aggressive management.
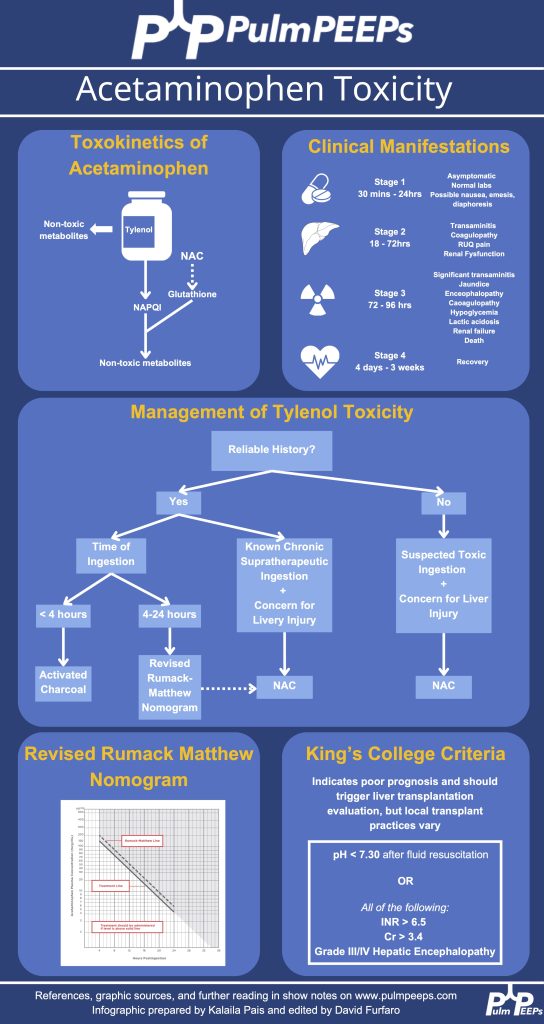
Tylenol Toxicity and Interpretation
- Pathophysiology:
- Tylenol overdose overwhelms liver glutathione, leading to accumulation of NAPQI, which causes hepatocyte necrosis.
- Interpretation of Tylenol Levels:
- Timing of ingestion is critical to interpreting levels.
- The Rumack-Matthew Nomogram is used for acute ingestions but requires a known ingestion time.
- Management:
- N-acetylcysteine (NAC): Standard of care; acts as a glutathione precursor and mitigates liver damage.
- Early use is recommended in suspected cases of Tylenol toxicity, even if ingestion timing is unclear.
Critical Management Principles
- Stabilization: Focus on airway, hemodynamics, and perfusion.
- Monitor for signs of cerebral edema (e.g., pupillary changes, seizures).
- In select patients, use hypertonic saline to maintain sodium levels (145–150 mmol/L) to mitigate cerebral edema risks.
- CRRT and Plasma Exchange:
- Continuous renal replacement therapy (CRRT) for hyperammonemia and acidosis.
- Plasma exchange (PLEX) may stabilize cytokine storms and improve survival.
- Organ-Specific Considerations:
- Renal failure: Common due to hepatorenal syndrome; requires CRRT.
- Coagulopathy: Managed with blood products as needed but indicates worsening liver synthetic dysfunction.
Prognosis and Transplant Considerations
- King’s College Criteria: Guides transplant listing for ALF patients.
- Factors: Encephalopathy severity, INR, lactate, bilirubin trends.
- Ethical considerations for liver transplant in patients with substance use or overdose:
- Emphasis on assessing social support and addressing psychiatric needs.
- Efforts are made to ensure equitable access to transplant when warranted.
Takeaways for Clinical Practice
- Broad Differential Diagnosis: Keep a wide perspective for acute liver presentations, considering toxins, infections, and systemic conditions.
- Early Use of NAC: Err on the side of initiating NAC when Tylenol toxicity is suspected.
- CNS Focus in ALF: Monitor and manage cerebral edema aggressively.
- CRRT & PLEX: Advanced liver support techniques are critical in select cases.
- Interdisciplinary Collaboration: Psychiatrists, neurocritical care, and hepatologists play pivotal roles in management.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More