Our episode today is diving into a broader initiative to discuss the management of interstitial lung disease. In this episode we will be talking about the treatment of Idiopathic Pulmonary Fibrosis through the lens of a journal club discussion of the NEJM 2014 INPULSIS trial. Today’s episode is hosted by Pulm PEEPs Associate Editor Luke Hedrick.
Meet Our Guests
Robert Wharton is a recurring guest on Pulm PEEPs as a part of our Rapid Fire Journal Club Series. He completed his internal medicine residency at Mt. Sinai in New York City, and is currently a first year pulmonary and critical care fellow at Johns Hopkins.
Dr. Nicole Ng is an Assistant Profess of Medicine at Mount Sinai Hospital, and is the Associate Director of the Interstitial Lung Disease Program for the Mount Sinai National Jewish Health Respiratory Institute.
Article and Reference
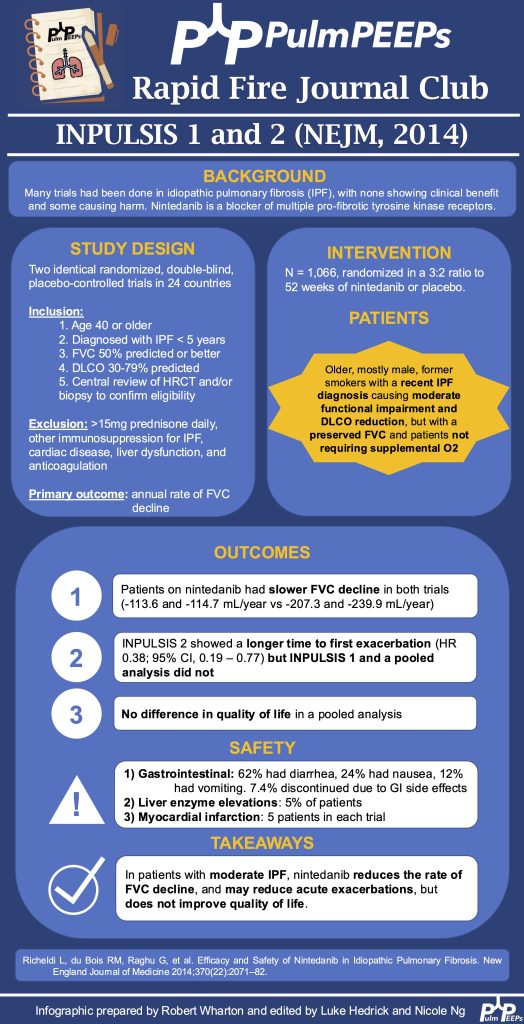
Today the discussion of IPF treatment centers around the 2014 NEJM publication of the INPULSIS trials investigating the efficacy of Nintedanib for the treatment of IPF.
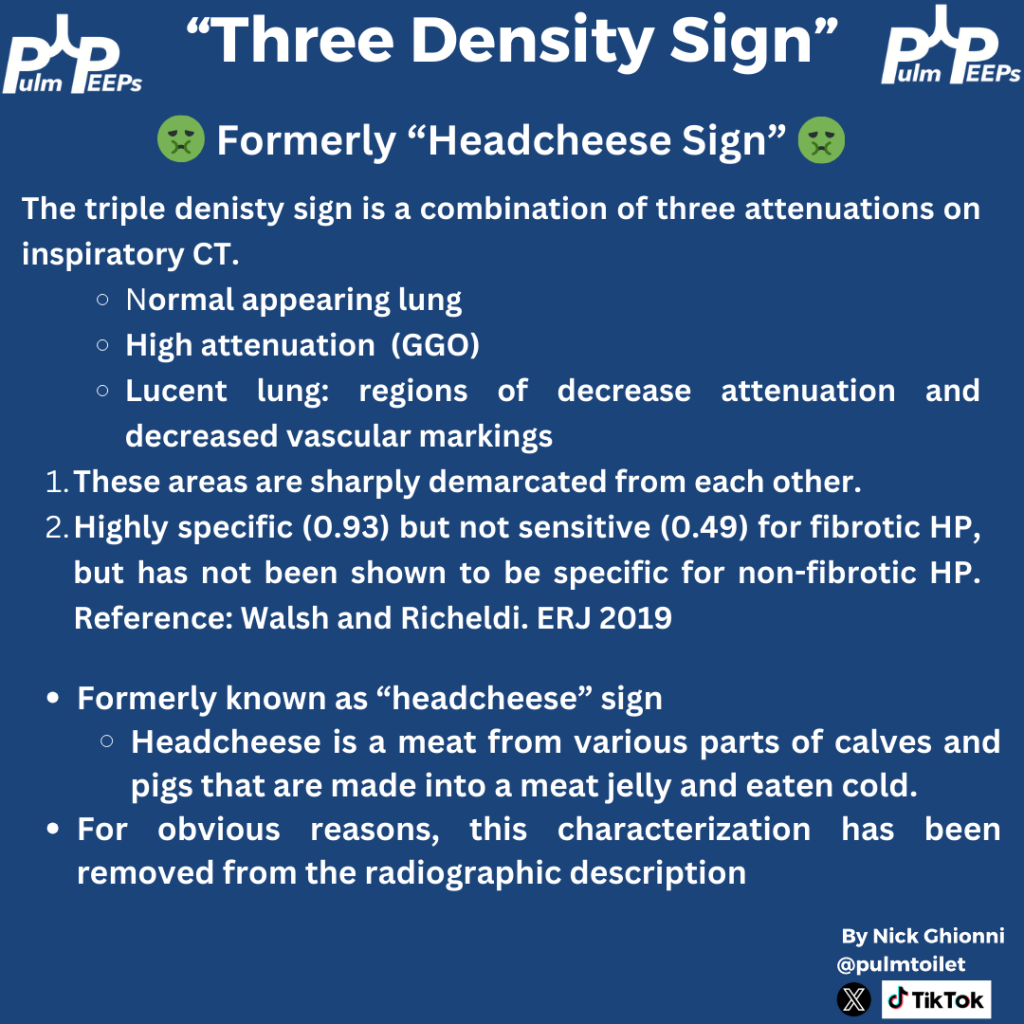
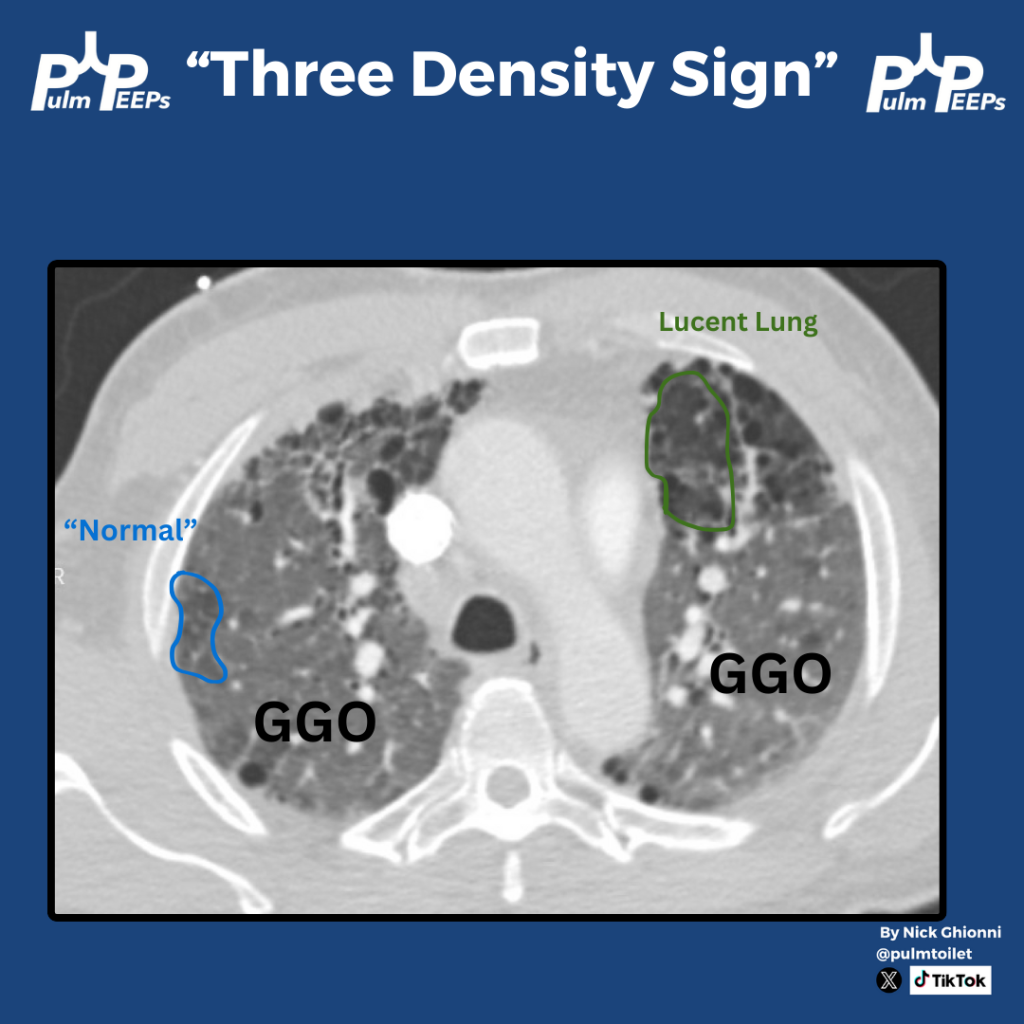
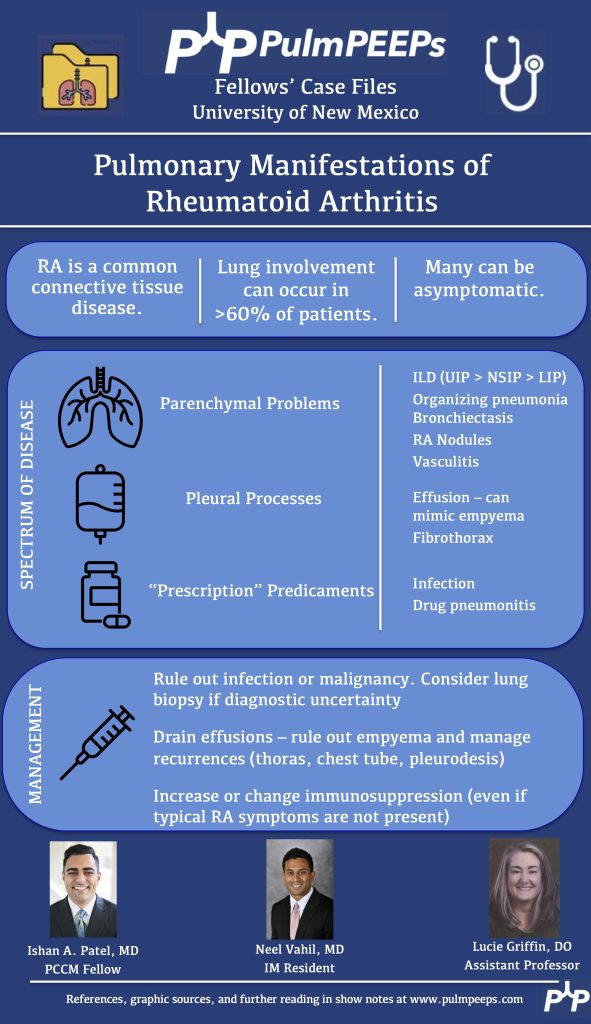
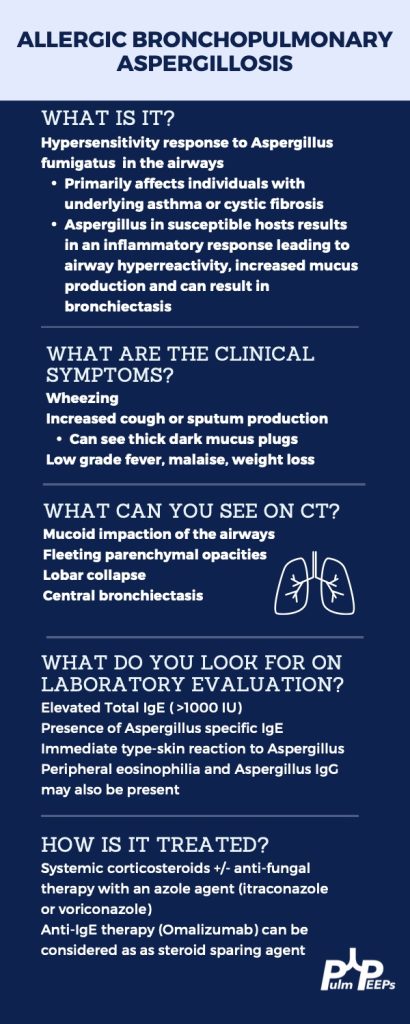
Infographic
Summary of Key Discussion Points
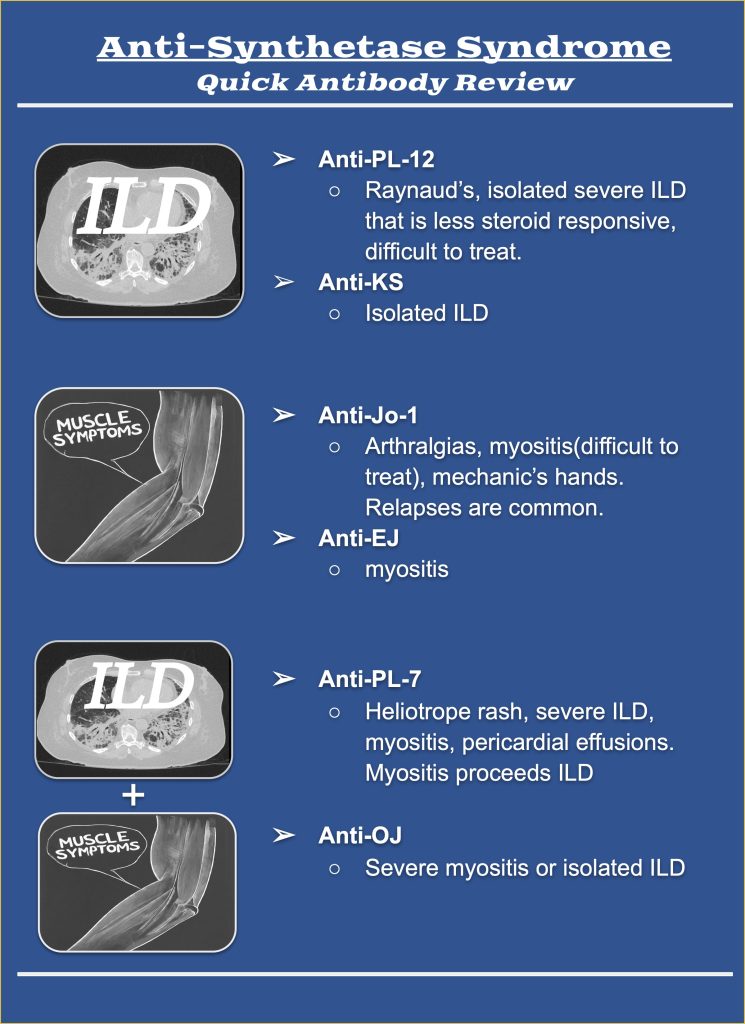
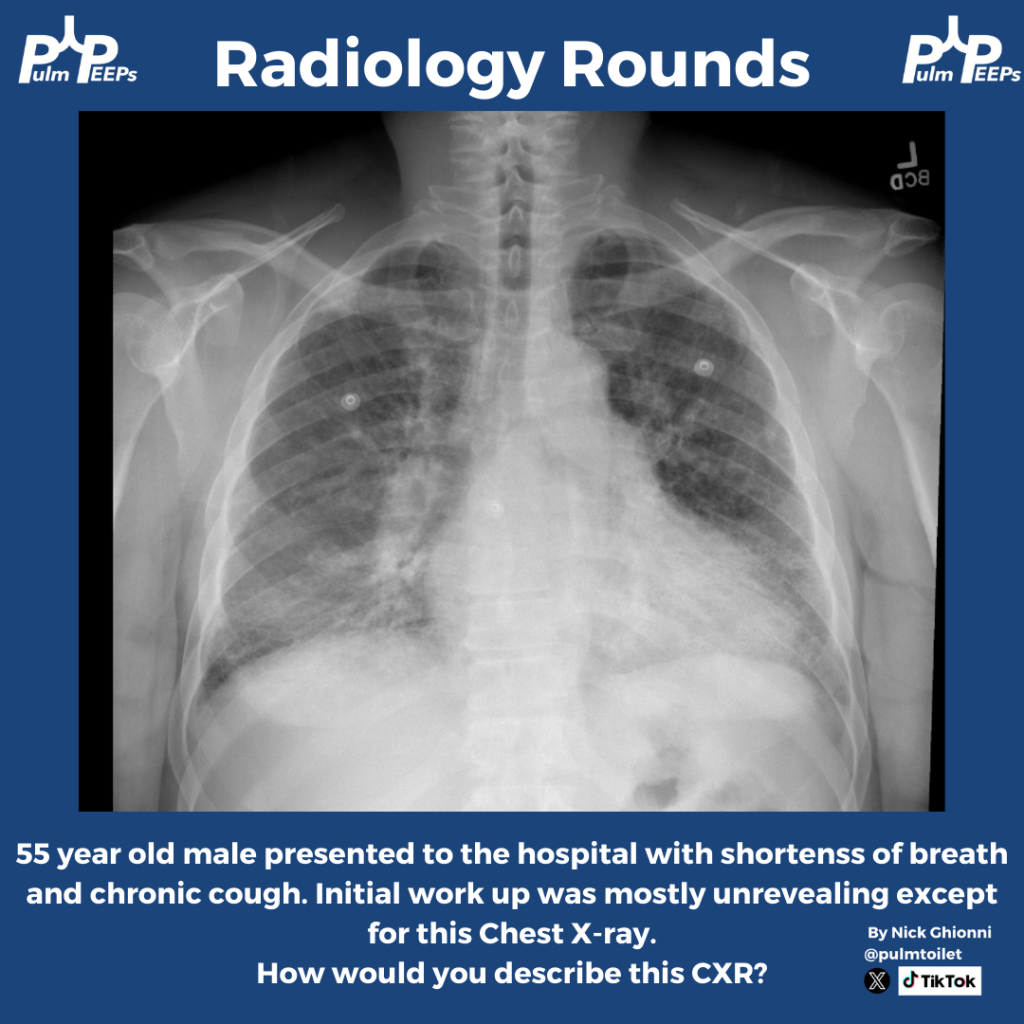
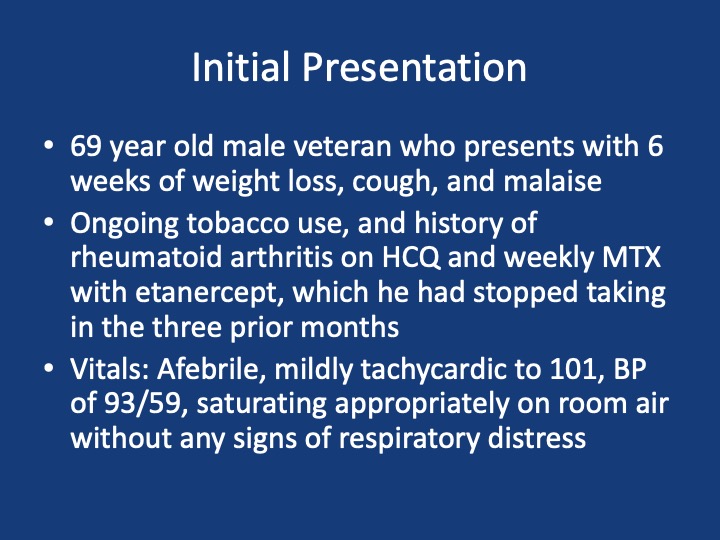
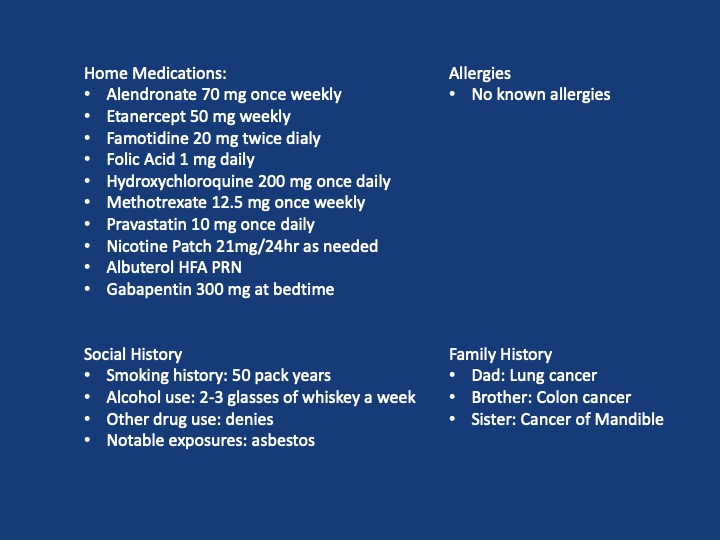
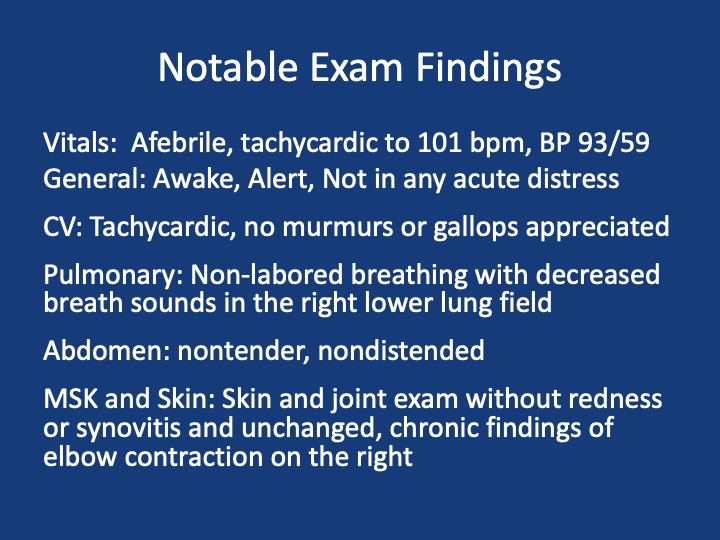
Background and Challenges in ILD Treatment: Interstitial lung diseases (ILDs), particularly idiopathic pulmonary fibrosis (IPF), had historically poor treatment outcomes, with numerous therapies showing either no benefit or even harm. Prior to 2014, effective treatments were extremely limited, and lung transplantation was the primary management option.
INPULSIS I and II Trials: These 2014 trials examined nintedanib, an antifibrotic drug initially tested for cancer, in patients with moderate IPF. The studies were well-structured, involving strict criteria to ensure accurate diagnoses and excluding younger patients or those with more advanced disease.
Nintedanib’s Mechanism and Design of the Trials: Nintedanib acts by blocking multiple tyrosine kinases that mediate fibrotic growth factors. Patients were monitored over a year, with primary endpoints focusing on forced vital capacity (FVC) decline—a common surrogate measure for disease progression in ILD trials due to its correlation with survival.
Outcomes: Both trials showed that nintedanib significantly reduced the rate of FVC decline compared to placebo, suggesting that it slowed disease progression. Secondary endpoints included reduced acute exacerbations (significant only in one trial) and minor improvements in quality of life, though these weren’t statistically or clinically significant.
Adverse Effects: Nintedanib’s side effects included gastrointestinal issues (diarrhea, nausea, vomiting) and, less commonly, liver enzyme elevations and cardiovascular events. While post-marketing data suggested some improvements in tolerability, clinicians still monitor for these side effects closely.
Application in Clinical Practice: The trials support nintedanib as an option for slowing IPF progression, though no cure or disease reversal is achieved. Clinicians weigh the choice between nintedanib and pirfenidone (another antifibrotic) based on each drug’s side effect profile and individual patient needs.
Future Directions: The trials paved the way for further research into multi-therapy approaches for ILD, targeting multiple disease pathways, similar to strategies in asthma or COPD. Upcoming therapies and trials aim to provide more targeted and effective options for IPF and other ILDs.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More