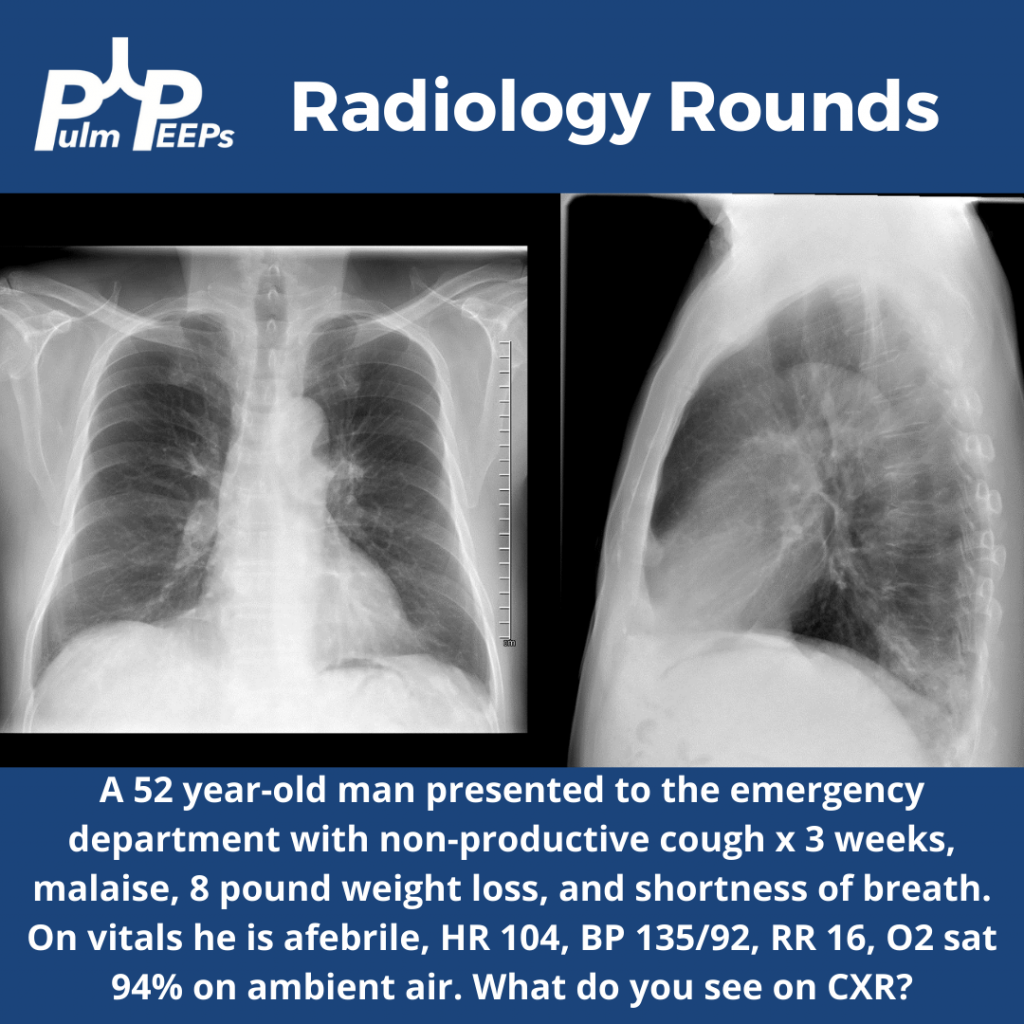
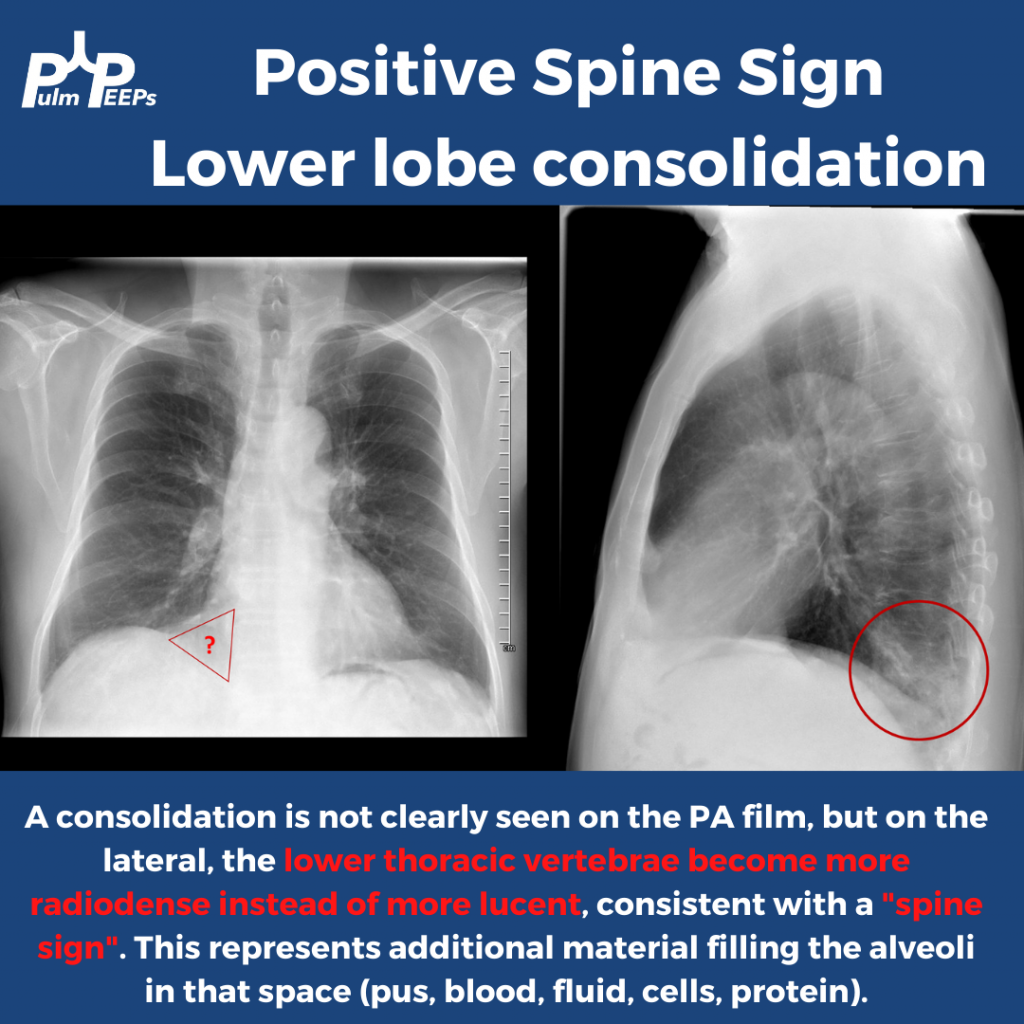
It is Tuesday and time for another #RadiologyRounds!! This is a patient who presented to the emergency department with symptoms of cough, dyspnea, malaise, and weight loss. A PA and lateral CXR was obtained.
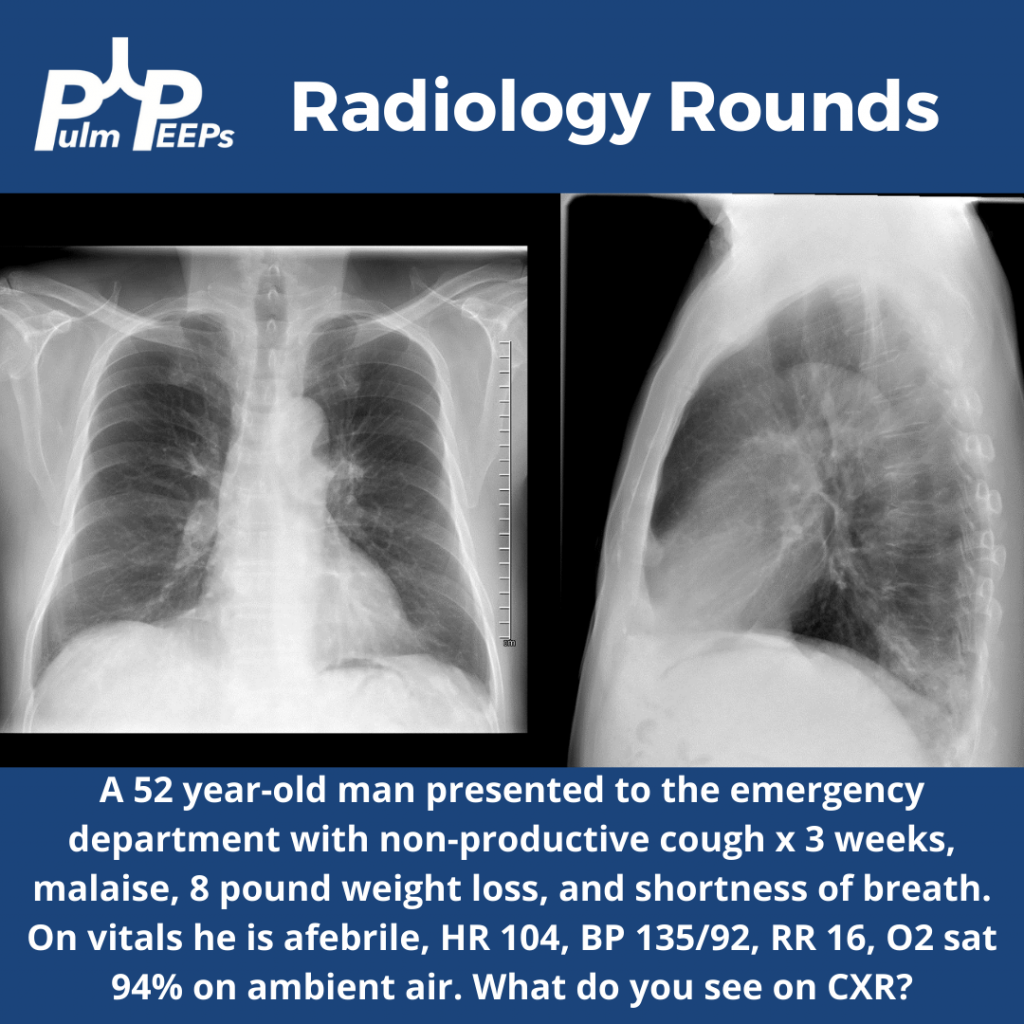
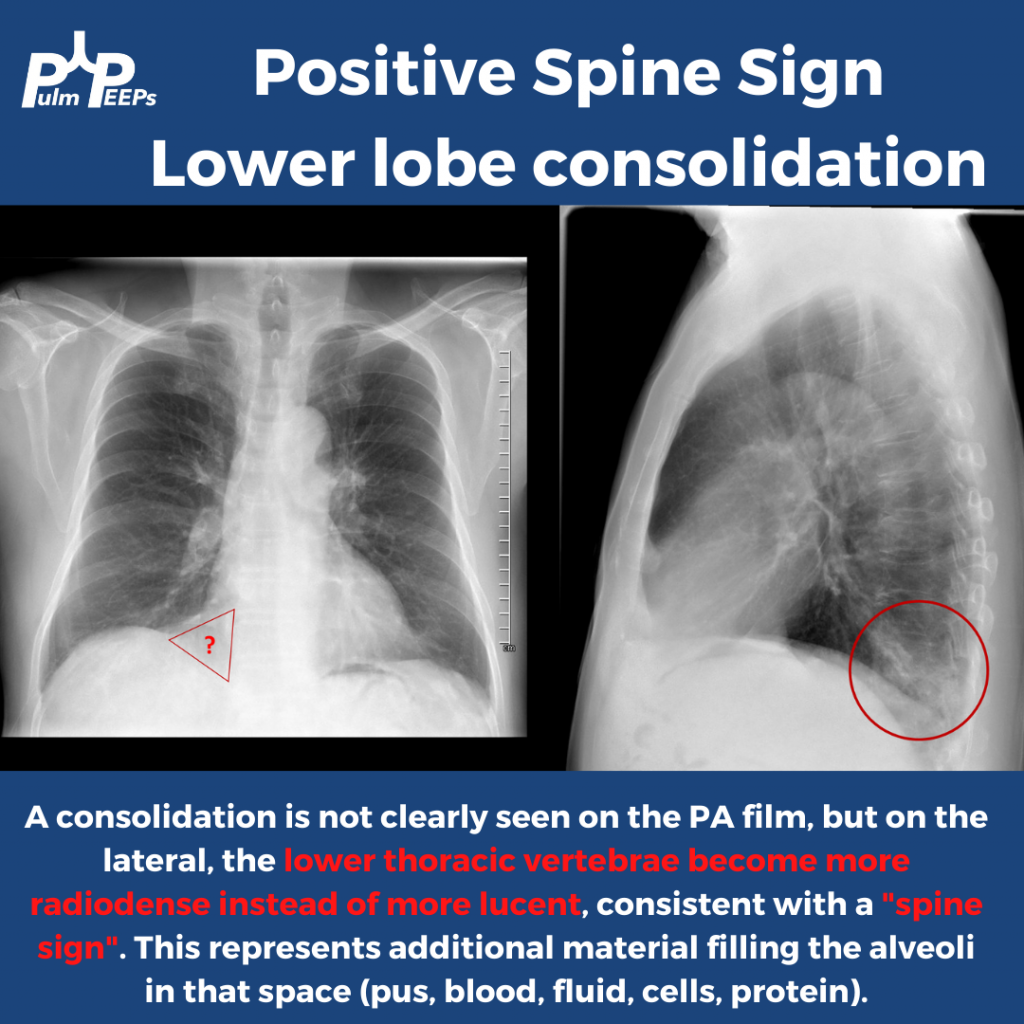

It is Tuesday and time for another #RadiologyRounds!! This is a patient who presented to the emergency department with symptoms of cough, dyspnea, malaise, and weight loss. A PA and lateral CXR was obtained.
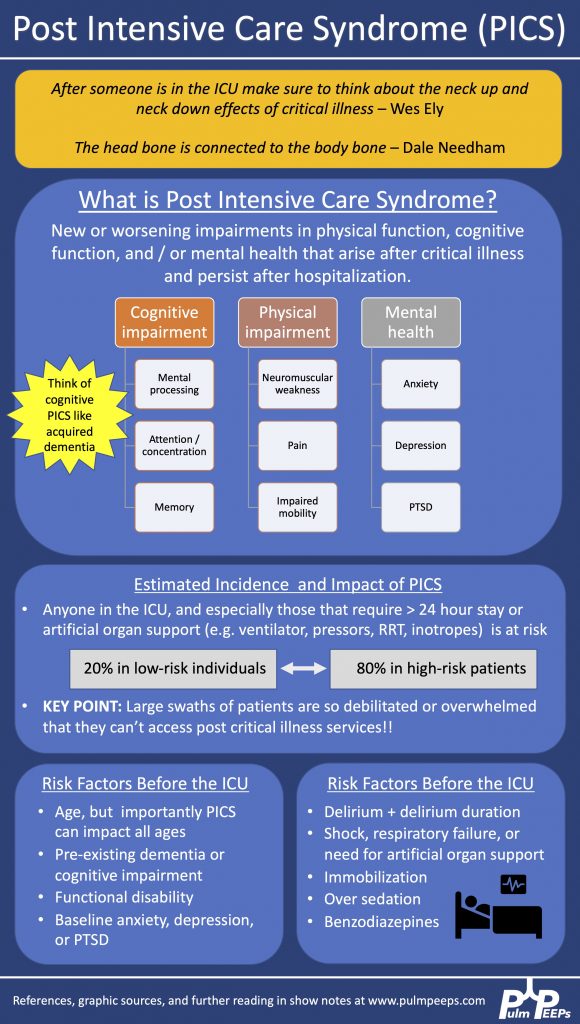
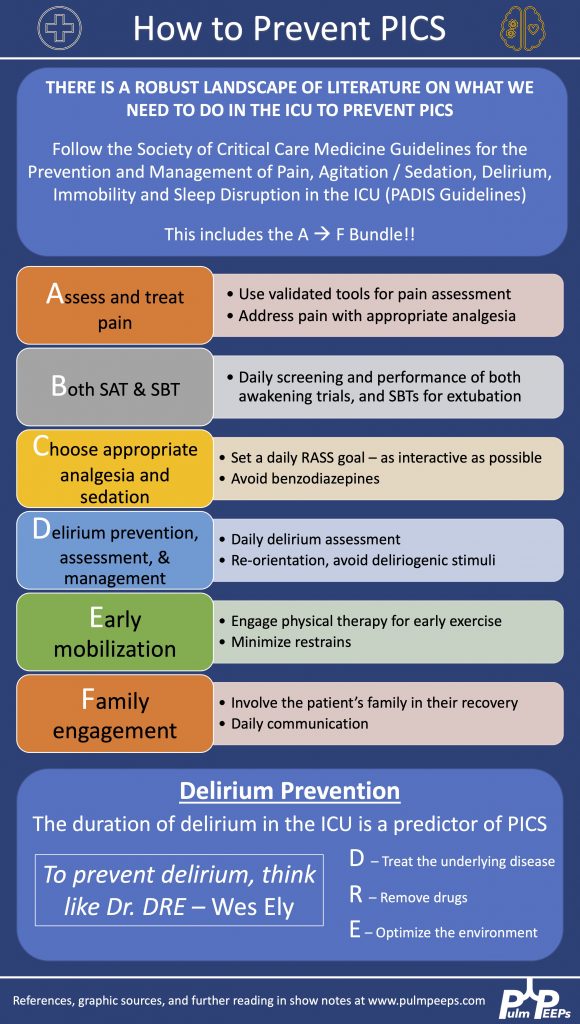
Today on Pulm PEEPs, we are joined by two pioneers in the field of post-intensive care outcomes and delirium research. Drs. Dale Needham and Wes Ely talk to us all about the Post Intensive Care Syndrome (PICS) and cover everything from how it was first recognized, to the impact it has, and, most importantly, what we can do to prevent it. This is a huge topic in the field of critical care and we’re thrilled to be delving into it with such knowledgeable guides.
Meet Our Guests
Wes Ely is the Grant W. Liddle Chair in Medicine and a Professor of Medicine at Vanderbilt University Medical Center. He is also the Associate Director of Aging Research at the VA Tennessee Valley Geriatric Research and Education Clinical Center and the co-director of the Critical, Illness, Brain Dysfunction and Survivorship Center. He has published 100s of manuscripts on critical illness survivorship and delirium. He also published a book called “Every Deep-Drawn Breath” about his and his patients’ experiences in the ICU and about the ramifications of critical illness. All net proceeds for the book are going to the CIBS Center Endowment for Survivorship
Dale Needham is a Professor of Medicine at Johns Hopkins, where he is also the Medical Director of the Critical Care Physical Medicine and Rehabilitation Program and the Director of the Outcomes After Critical Illness and Surgery Group. He is the author of 100s of publications focusing on post-ICU outcomes and has received numerous research grants from the NIH and other organizations.
Key Learning Points
Visit our website www.pulmpeeps.com to see the key learning points from this episode summarized in two infographics.
References and links for further reading
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
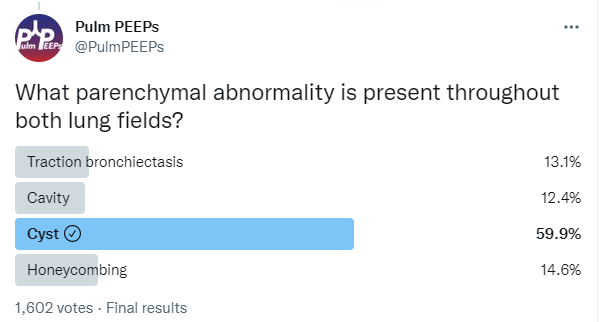
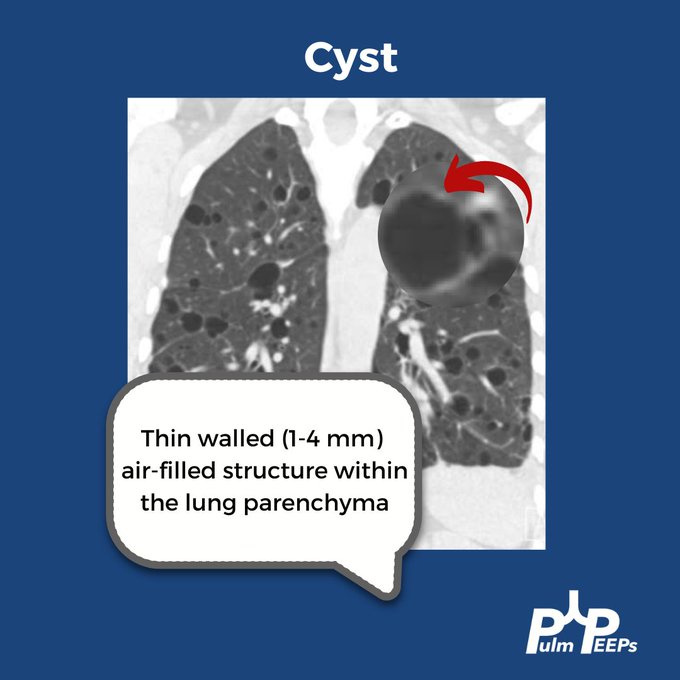
Time for another #RadiologyRounds!! This week we’re looking at the coronal CT scan views, which can be extremely helpful and are often under-utilized. Follow us on Twitter to work through Radiology Rounds cases as they come out.
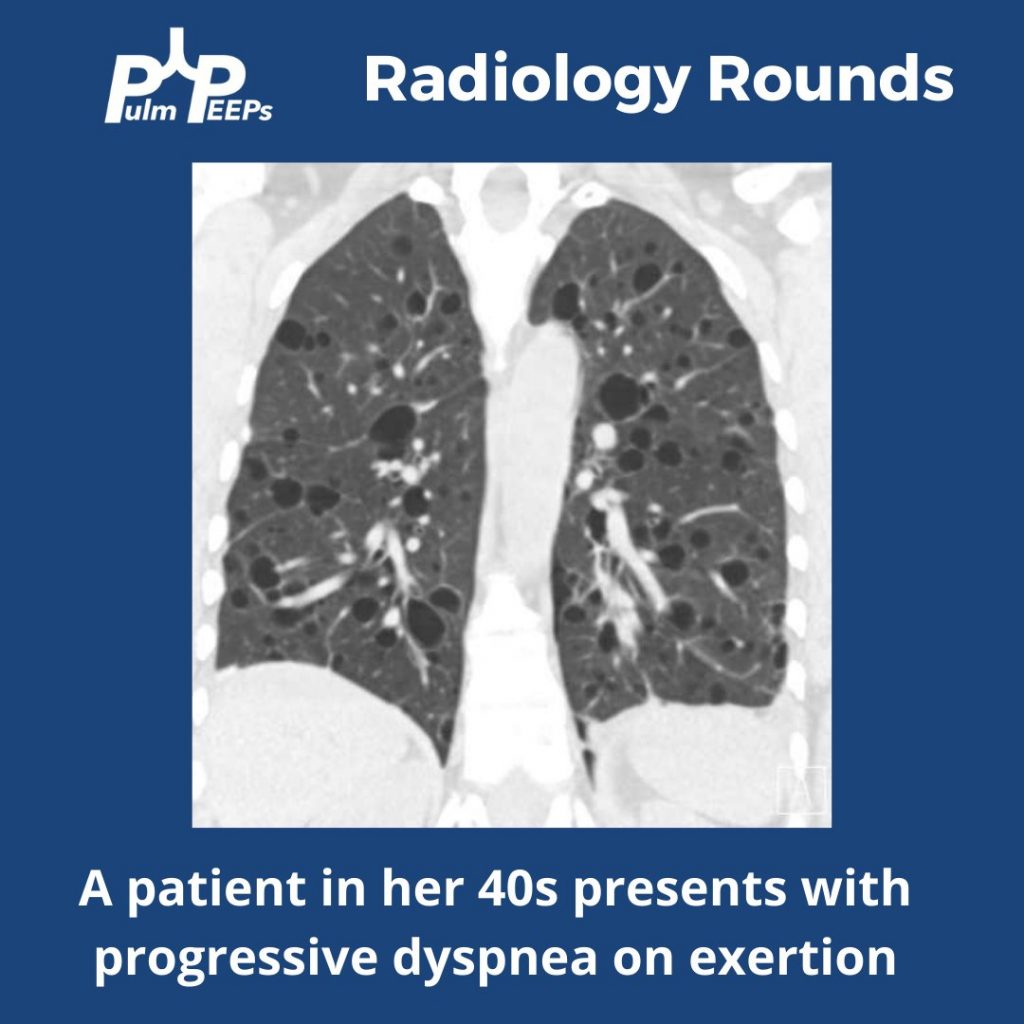
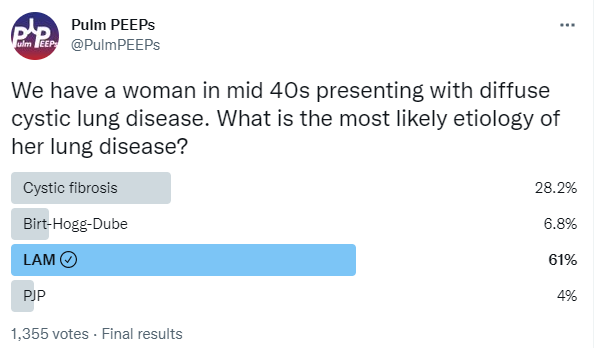
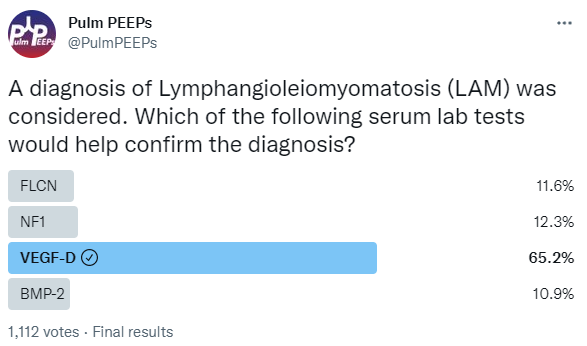
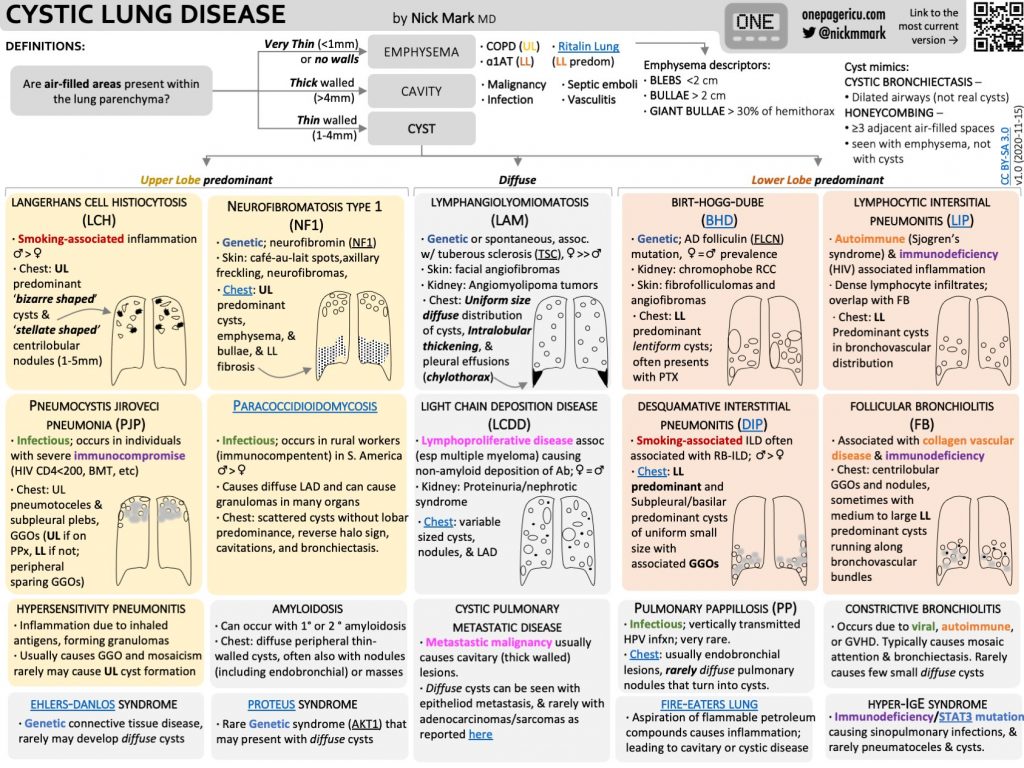
Our patient had an elevated VEGF-D level, a renal angiomyolipoma identified on CT abdomen, and imaging with diffuse cystic lung disease confirming her diagnosis of LAM. Make sure to check out the ICUOnePager made by Dr. Nick Mark.
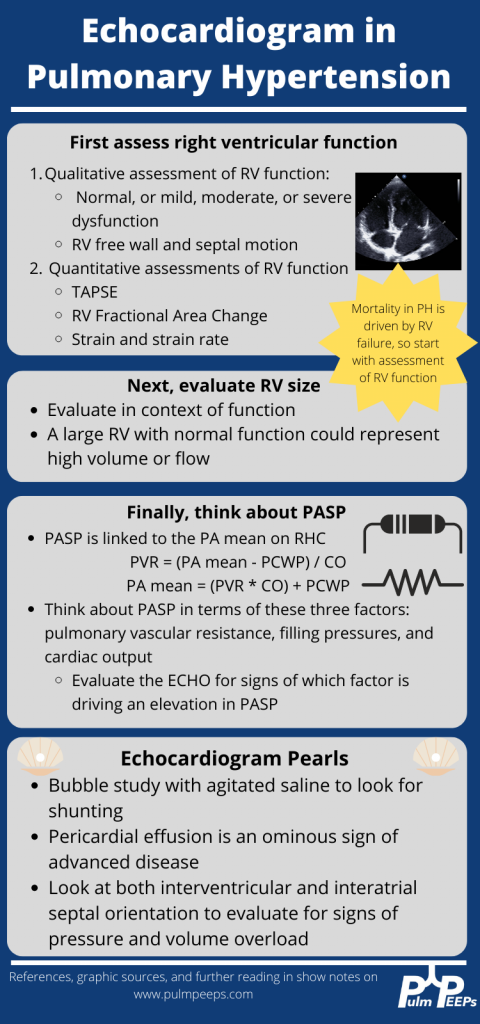
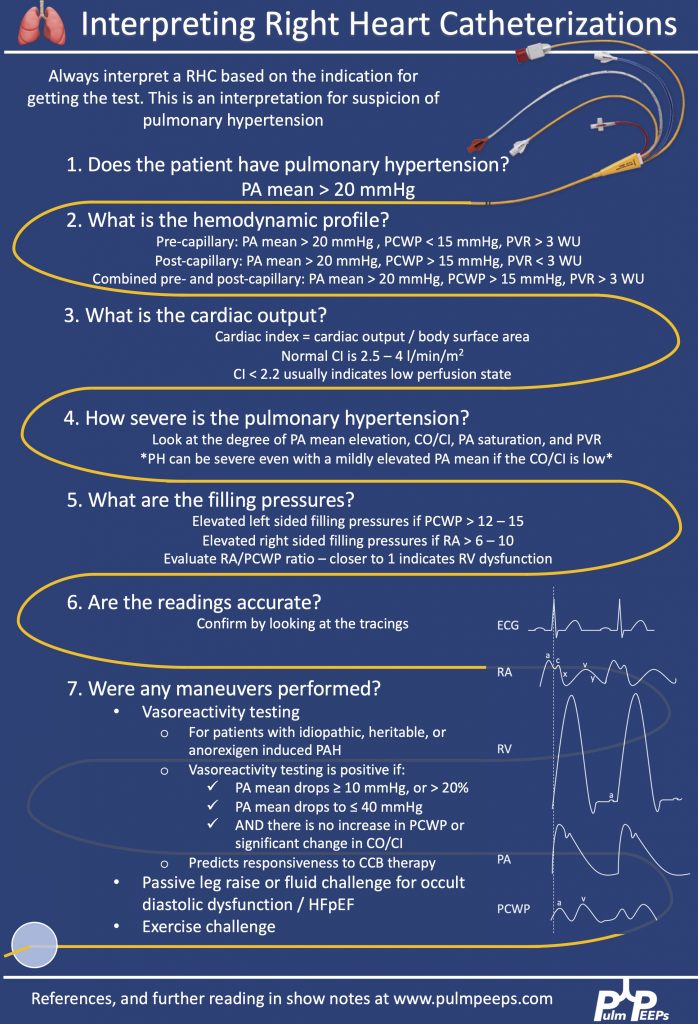
This week on Pulm PEEPs, we are continuing our Top Consults series with a discussion on the work-up and diagnosis of Pulmonary Hypertension. See our prior Radiology Rounds on signs of PAH on CT scan, and listen to our follow-up episode on right heart catheterizations for some background before this episode… or dive right in! We’ll cover everything from history and physical, to recent guideline changes in the definition of PH, and much, much more!
Meet Our Guests
Erika Berman Rosenzweig is a Professor of Pediatrics and the Director of the Pulmonary Hypertension Center and CTEPH Program at Columbia University Medical Center / New-York Presbyterian Hospital. She is an active member of the Pulmonary Hypertension Association, was the Editor-in-Chief of Advances in Pulmonary Hypertension and is on the Scientific Board of the World Symposium on PH.
Catherine Simpson is an Assistant Professor of Medicine at Johns Hopkins Hospital and is one of the faculty members in our Pulmonary Hypertension group. Her clinical and research areas of expertise are in pulmonary vascular disease and right heart function. Her research is focused on novel biomarker discovery and metabolomics in pulmonary vascular disease.
Cyrus Kholdani is an Instructor in Medicine at Beth Israel Deaconess Medical Center and Harvard Medical School. He is also the director of the Pulmonary Hypertension Program at BIDMC, and is actively involved in clinical care and clinical research in a variety of pulmonary vascular disease domains.
Consult Patient
Ms. Pamela Harris (PH) is a 47-year-old woman with PMH of migraines, obesity s/p gastric sleeve (BMI now 33), and a history of remote DVT in her 20s while on OCP s/p 6 months of AC who is referred to pulmonary hypertension clinic for evaluation of dyspnea on exertion. She has actually had dyspnea for some time and previously it has been attributed to her weight. Based on this, she pursued a gastric sleeve and has lost 55 pounds, but continues to have shortness of breath. She has no cough, and does not get dyspnea at rest, but notes that after 1 flight of stairs, or 2-3 blocks on flat ground she has shortness of breath. She saw her PCP and had basic labs, basic spirometry, and an echocardiogram. He did not note anything significant on examination in the notes.
The labs had no anemia, and normal renal and liver function. Her serum bicarbonate was 25 and there was no blood gas. Spirometry showed an FVC 82% predicted, FEV1 83% predicted, and FEV1/FVC was 99% predicted. The echocardiogram had normal LVEF, mild LVH, normal RV size and function qualitatively. There was mild TR with tricuspid valve peak regurgitant velocity of 3.4 m/sec. The estimated PASP + RA pressure (based on normal IVC diameter 2.1 cm) was 46 mmHg.
RHC: Systemic BPs 140s/90s, with O2 saturations 97-98% on RA throughout. RA mean pressure was 9, RV was 48 with an RVEDP of 17, PA was 48/27 with mean of 34, and PCWP mean was 11. CO/CI by Fick was 5.56 / 2.42, and by thermo was similar, 5.8 / 2.52. Her PA sat was 62%, and PVR was 3.97 WU.
Key Learning Points
History
Physical Exam
Work up for etiology of PH
References and links for further reading
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
This week’s #RadiologyRounds is brought to you by our newest Contributor, Matthew Tsai! Matt will be continuing to work with us to bring you great cases and images and we are thrilled to have him on the team! Follow us on Twitter and Instagram for our Radiology Rounds, podcast episode releases, and more!
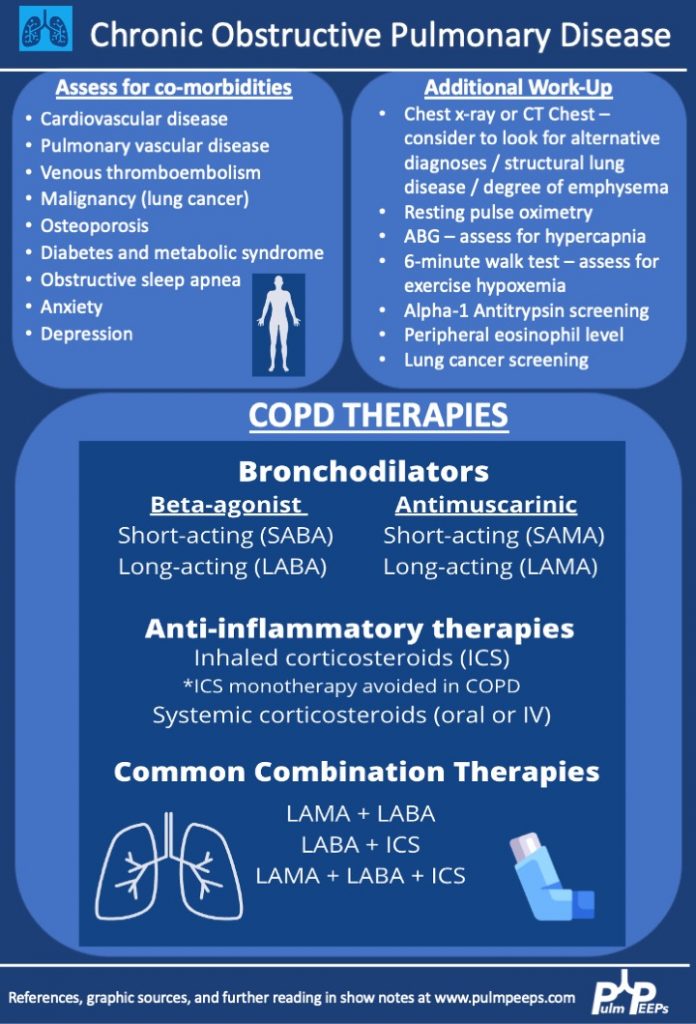
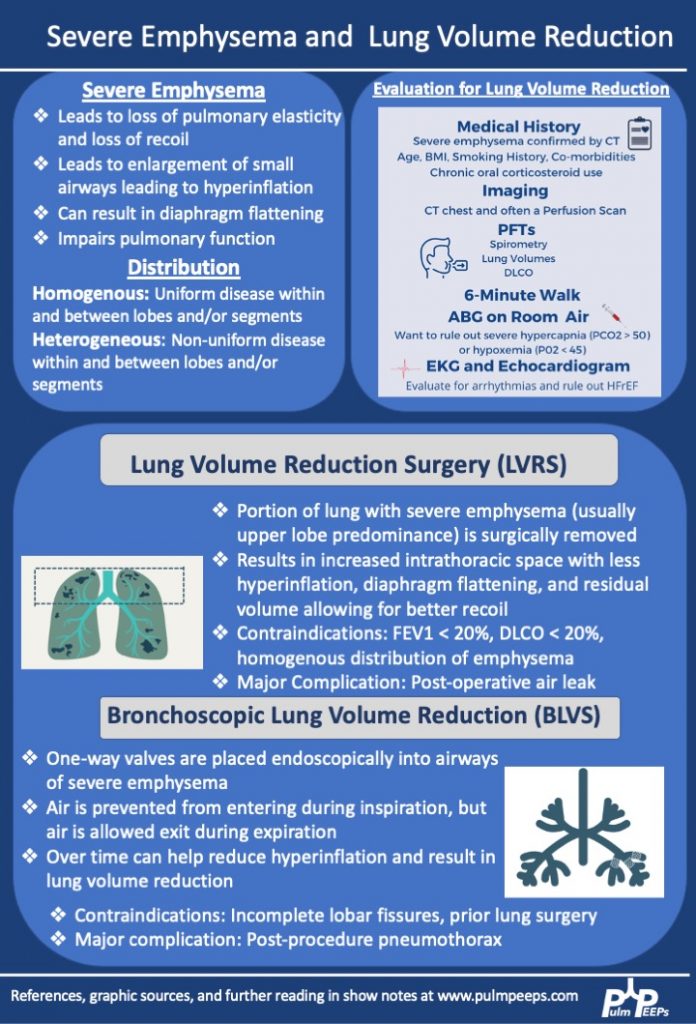
We are extremely excited for the third and final installment in our Pulm PEEPs and ATS Clinical Problems Assembly collaborative series on COPD. Today, we are joined by Drs. Jessica Bon, Michael Lester, and Niru Putcha to discuss severe COPD management and the role of lung volume reduction procedures. If you missed the first two parts of our series, make sure to check out episode 1 on COPD diagnosis and initial management, and episode 2 on COPD exacerbations.
Meet our Guests
Jessica Bon is an Associate Professor of Medicine at the University of Pittsburgh School of Medicine where she is also the Program Director for the Pulmonary and Critical Care Medicine Fellowship. Her research and clinical interests focus on lung disease progression in COPD and she manages patients with difficult-to-treat and severe COPD and evaluates patients for lung volume reduction surgery. Jessica was the chair of the ATS Clinical Problems Assembly Programming Committee from 2021 – 2022.
Michael Lester is an Assistant Professor of Medicine at Vanderbilt University Medical Center. Michael’s interests span both pulmonary and critical care medicine. He specializes in patients with advanced COPD and evaluation for bronchoscopic lung volume reduction surgery.
Niru Putcha is an Associate Professor of Medicine at Johns Hopkins School of Medicine and is an integral member and mentor in the Obstructive Lung Disease Group. Her research and clinical interests focus on the role of comorbidities on clinical outcomes in individuals with COPD. She also manages patients with difficult-to-treat and severe COPD and evaluates patients for lung volume reduction surgery. Niru is also the new chair of the ATS Clinical Problems Assembly Programming Committee.
Key Learning Points
Patients with advanced COPD should also be considered for lung transplantation. We will have an episode on lung transplant coming up soon!
References
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
This week on #RadiologyRounds we are extremely excited to share a case brought to you by one of our new Associate Editors, Leon Mirson! Enjoy, and follow us on Twitter and Instagram for content delivered to you weekly!
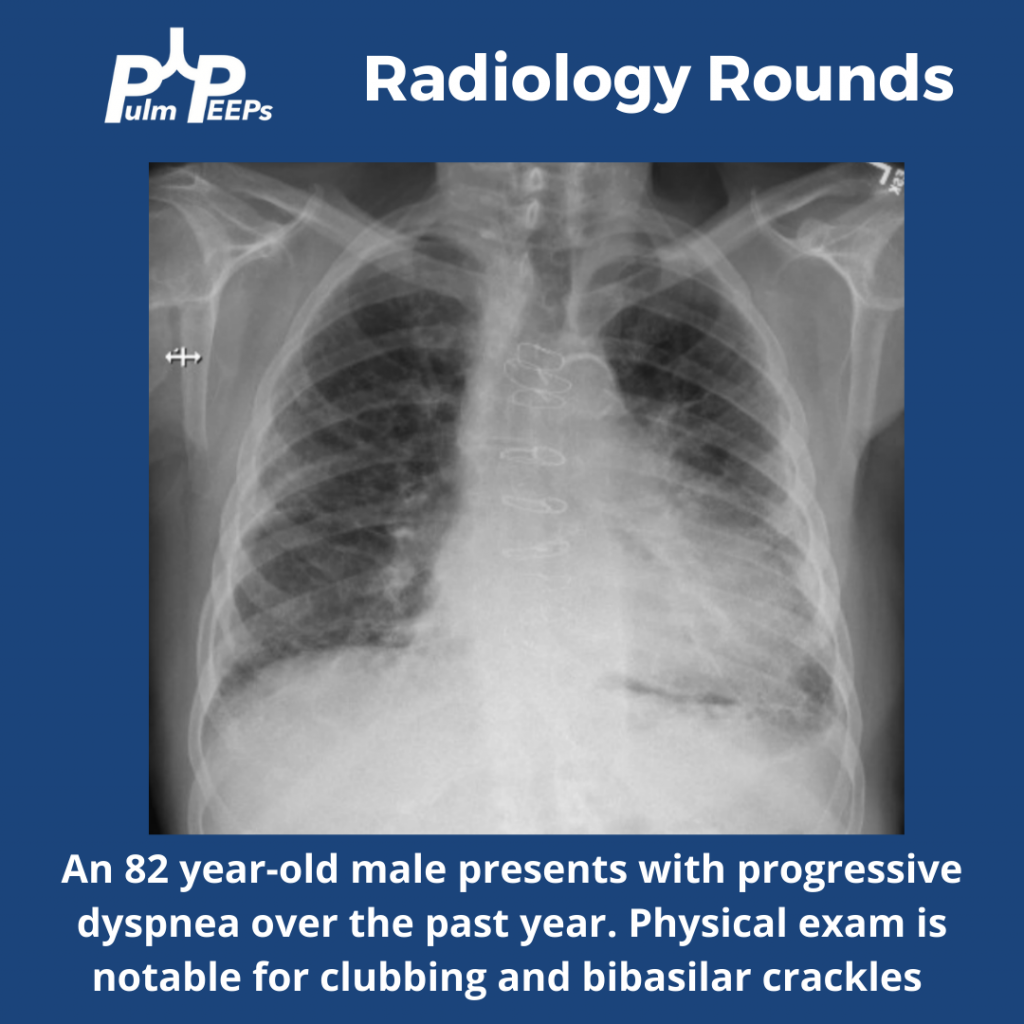
What abnormalities do you see on this CXR to help explain the patient’s presentation?
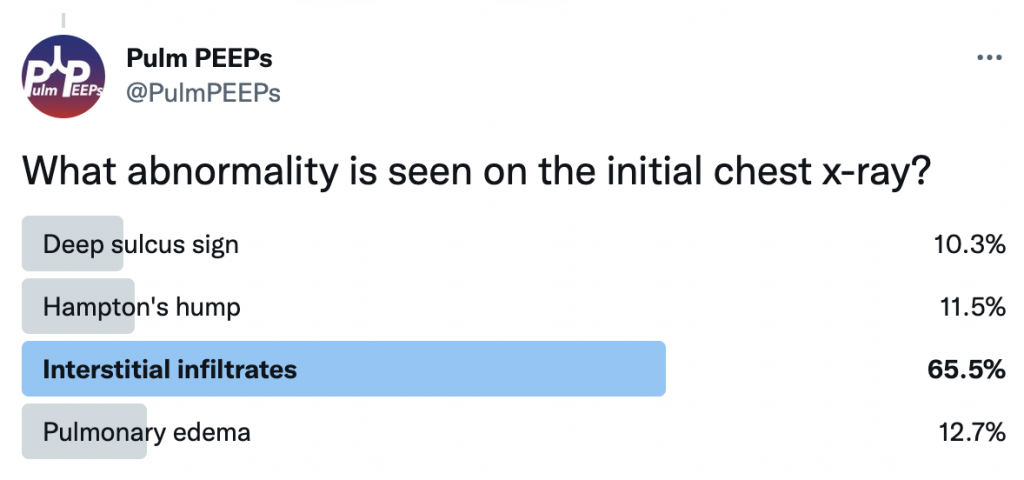
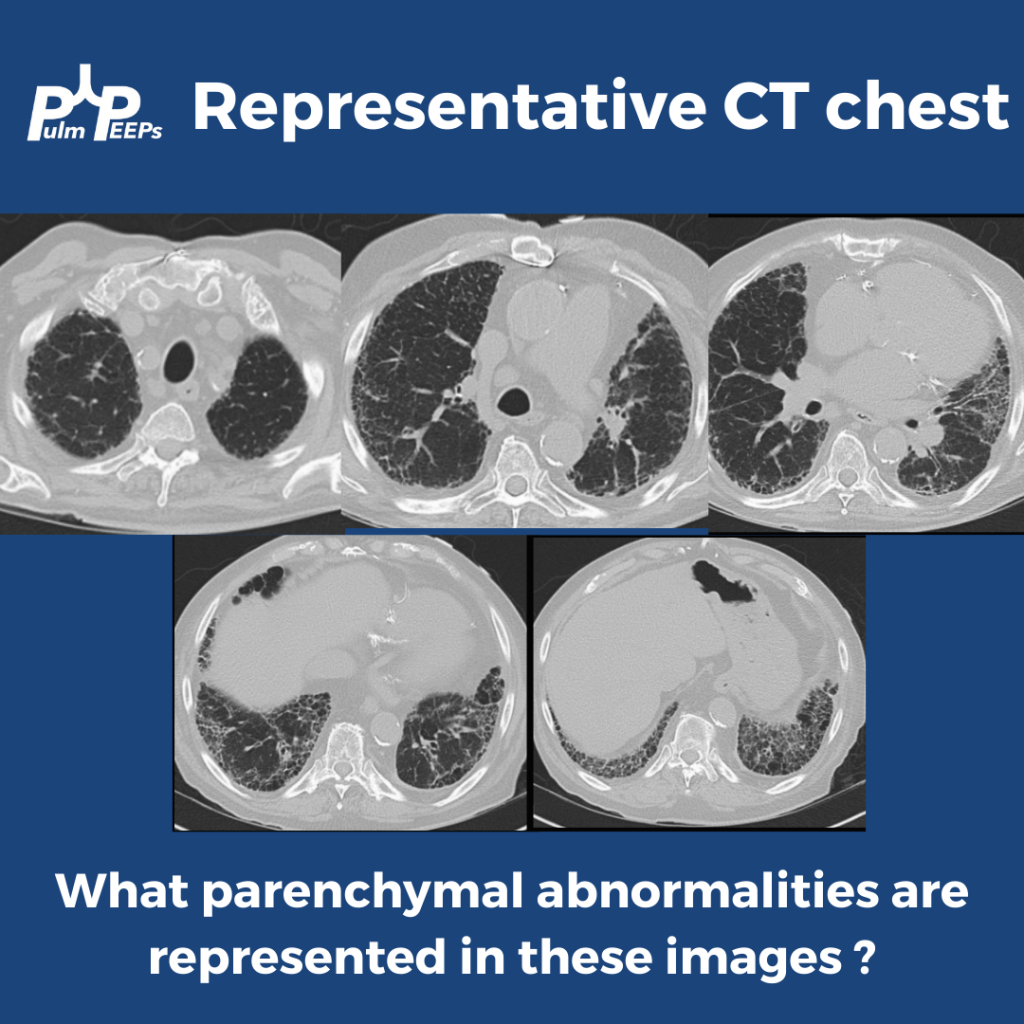
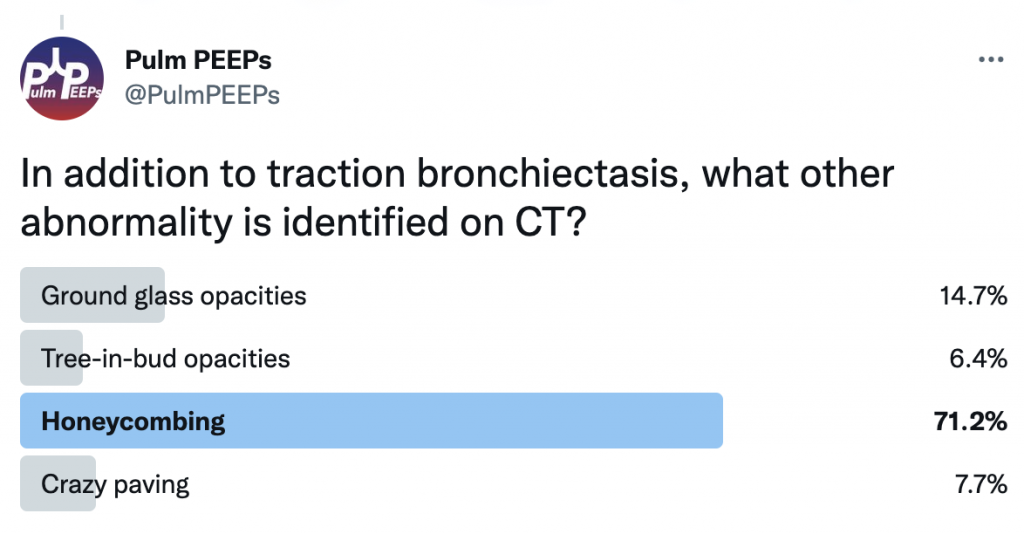
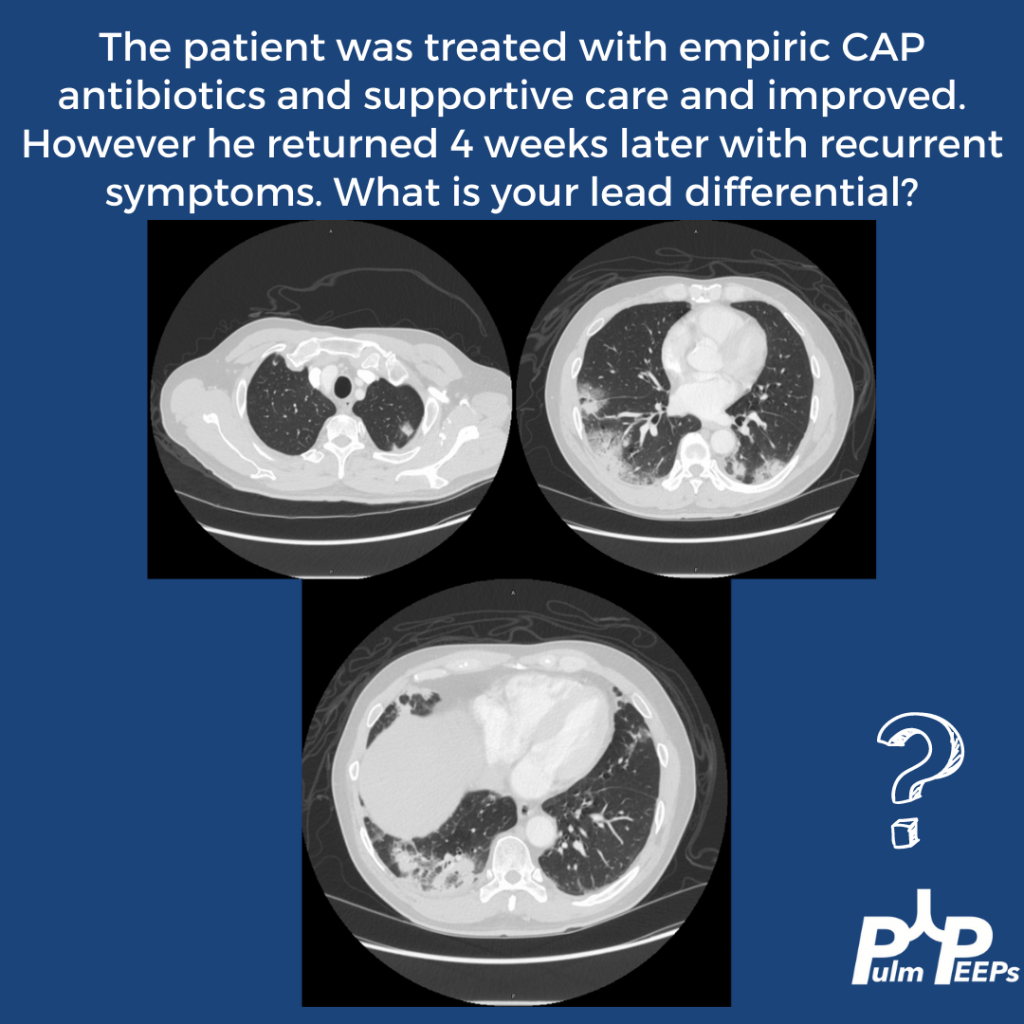
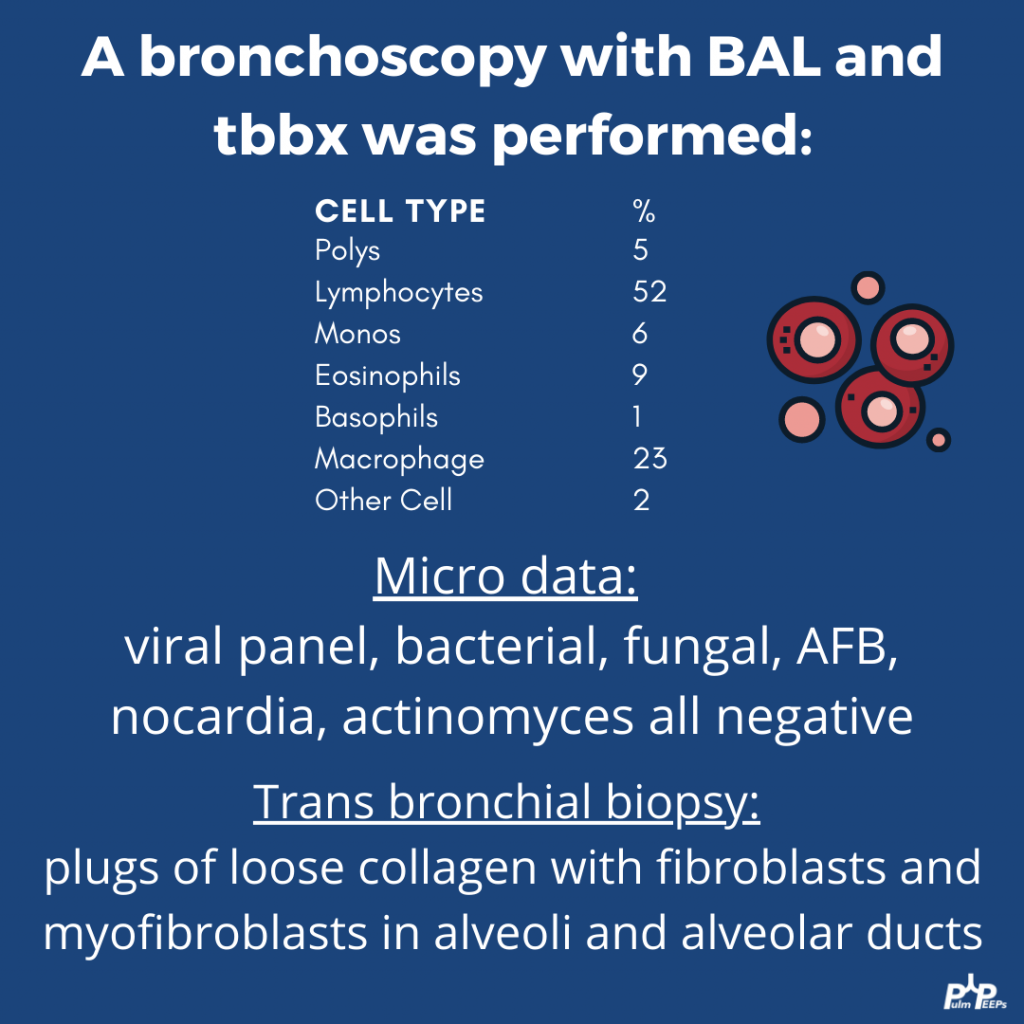
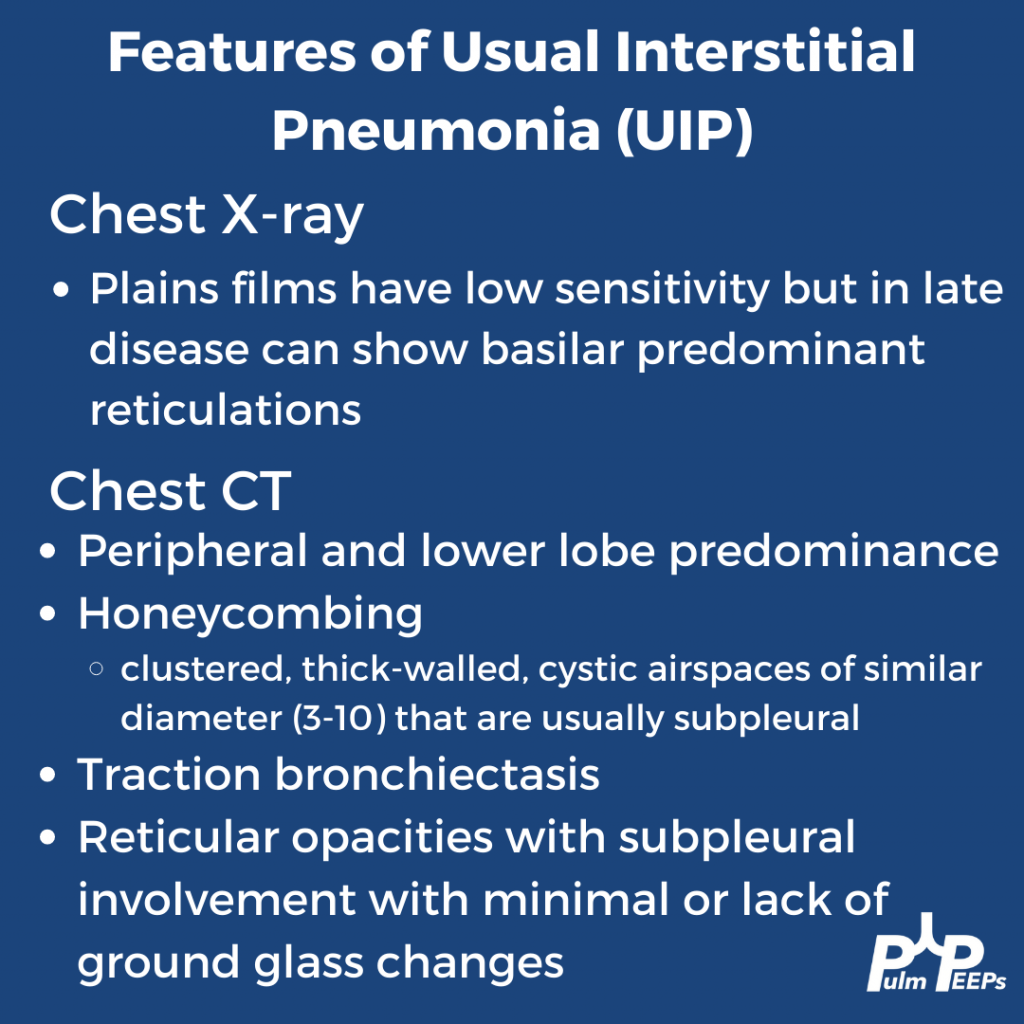
The CT scan has reticular changes consistent with interstitial lung disease and there are multiple features that help us define the pattern of the ILD. His CT notably has very few ground-glass opacities, there is traction bronchiectasis, and honeycombing with a basilar and peripheral / sub-pleural predominance.
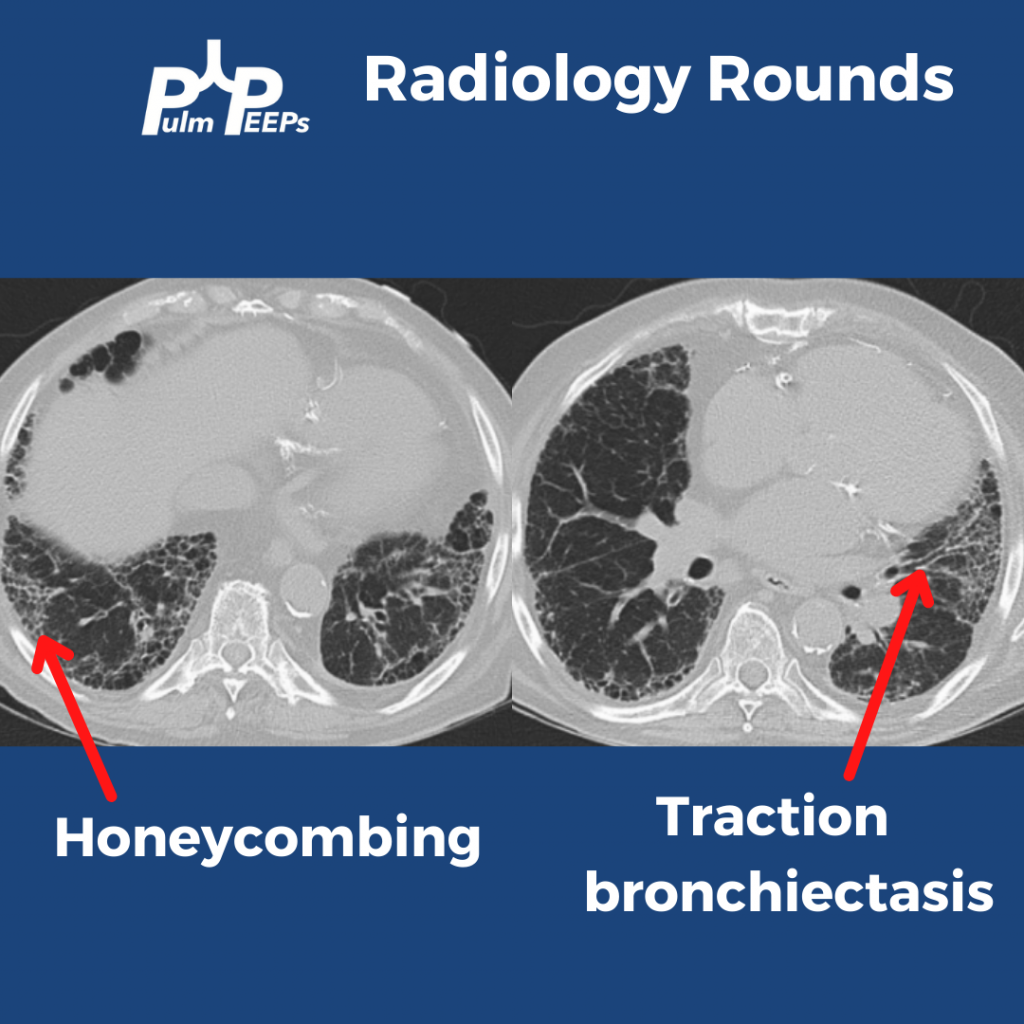
Taking all these features together, the patient’s radiographic presentation is consistent with Usual Interstitial Pneumonia (UIP)
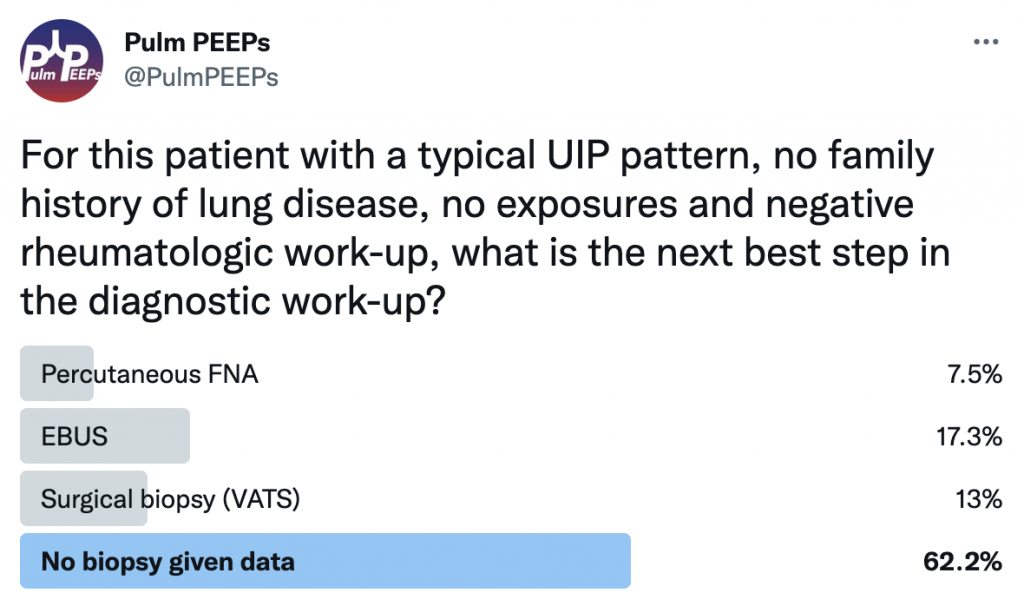
This patient had a thorough history taken and he had no prior smoking and no occupational or environmental exposures of significance. He had no family history of interstitial lung disease. A broad history was taken regarding symptoms of connective tissue disease and a broad serologic workup was sent, all of which were unremarkable. What would you want to do next diagnostically?
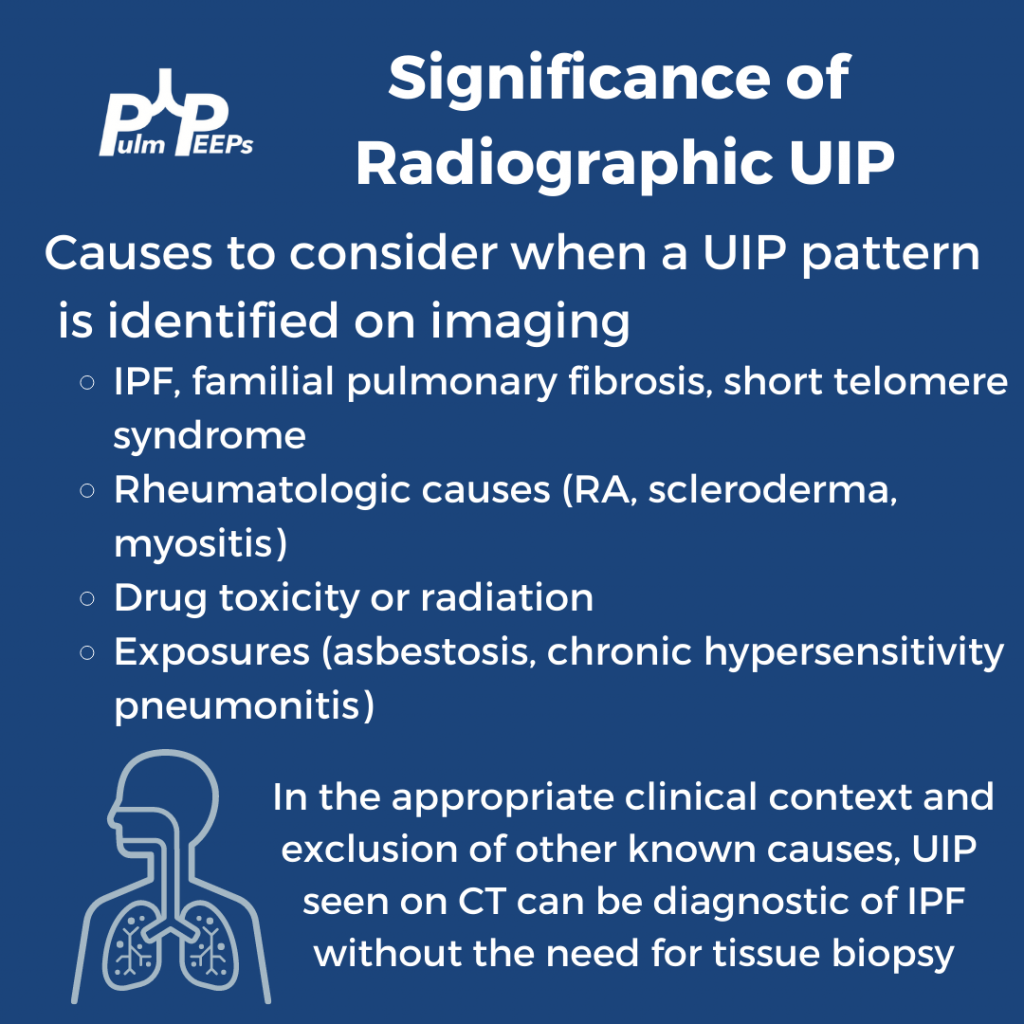
If you want to learn more about diagnosing interstitial lung disease, listen to our prior Top Consults episode on diagnosing ILD with experts in the field and see these prior #RadiologyRounds on Fibrotic NSIP and Sarcoidosis.

We are thrilled here @PulmPEEPS to have our first episode with one of our new Associate Editors Luke Hedrick, and our first nephrology consultant Jeff William. Luke will walk us through an interesting case presentation, and we will discuss an approach to severe weakness in our patient in the ICU.
Meet Our Guests
Jeff William is an Assistant Professor of Medicine at Harvard Medical School and Beth Israel Deaconess Medical Center, where he is also the Associate Director of the Nephrology Fellowship Program. He completed a Medical Education Research Fellowship at Harvard Medical School, and is very involved in residency, fellowship and medical student education.
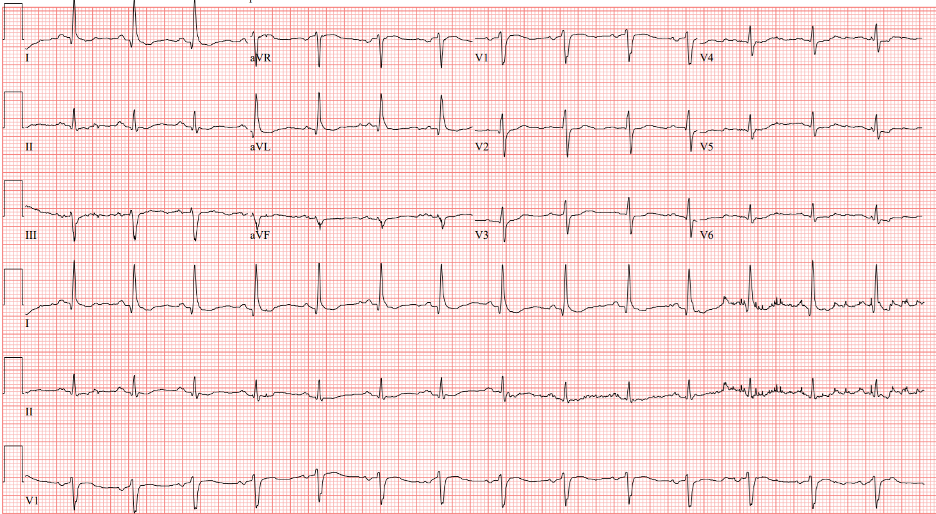
Patient Presentation
We have a man in his 40s with a past medical history of asthma, hypertension, and acid reflux who was brought in by EMS with back pain and profound proximal lower extremity weakness. He reports mild weakness in his legs which started 2 days ago, but this morning his weakness acutely worsened to the point that he can’t lift his legs out of the bed. He also has some cramping pain in his thighs. He additionally has had mild shortness of breath and yesterday went to an urgent care where he was given steroids and swabbed for COVID (which was negative).
**Spoilers Ahead** If you want to think through the case on your own we advise listening to the episode first before looking at the infographics below
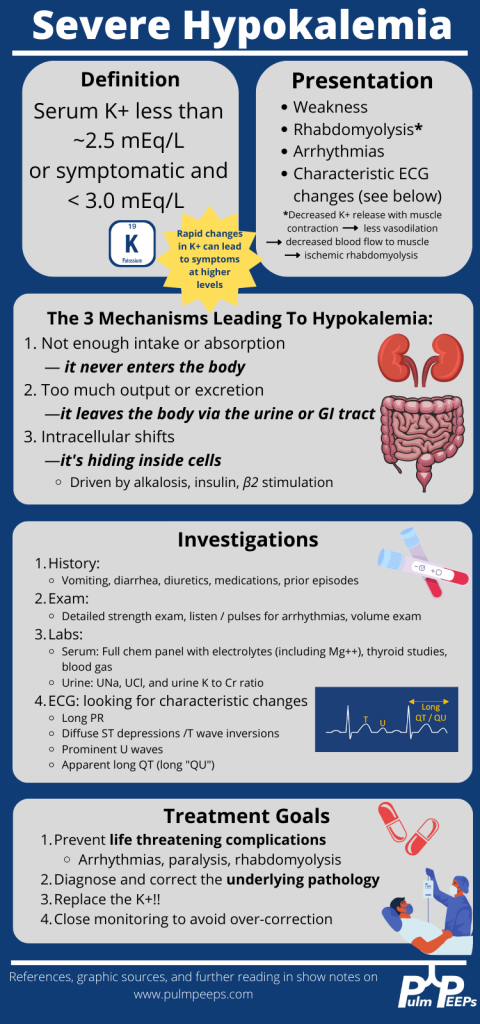
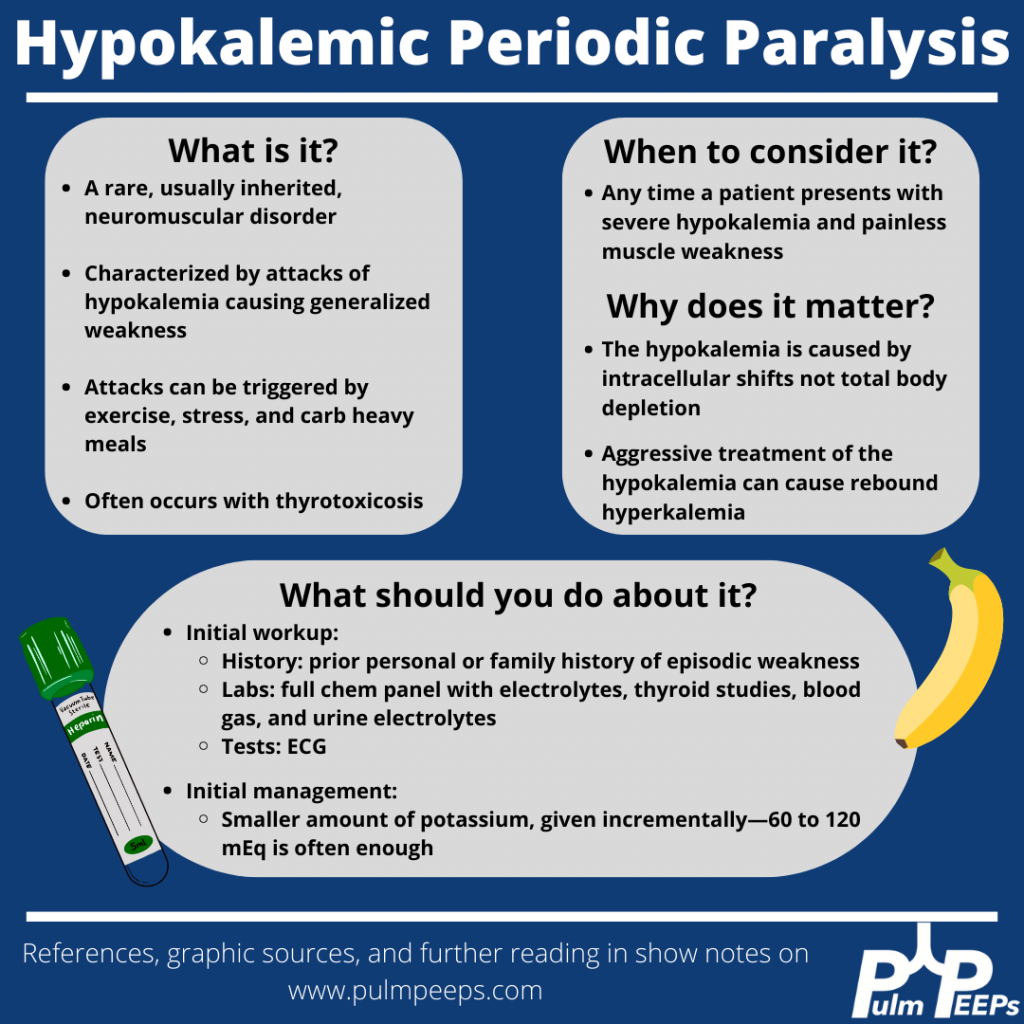
Although our patient’s etiology of severe hypokalemia was thought to be secondary to thiazide diuretic use, it is important to be familiar with hypokalemic periodic paralysis.
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
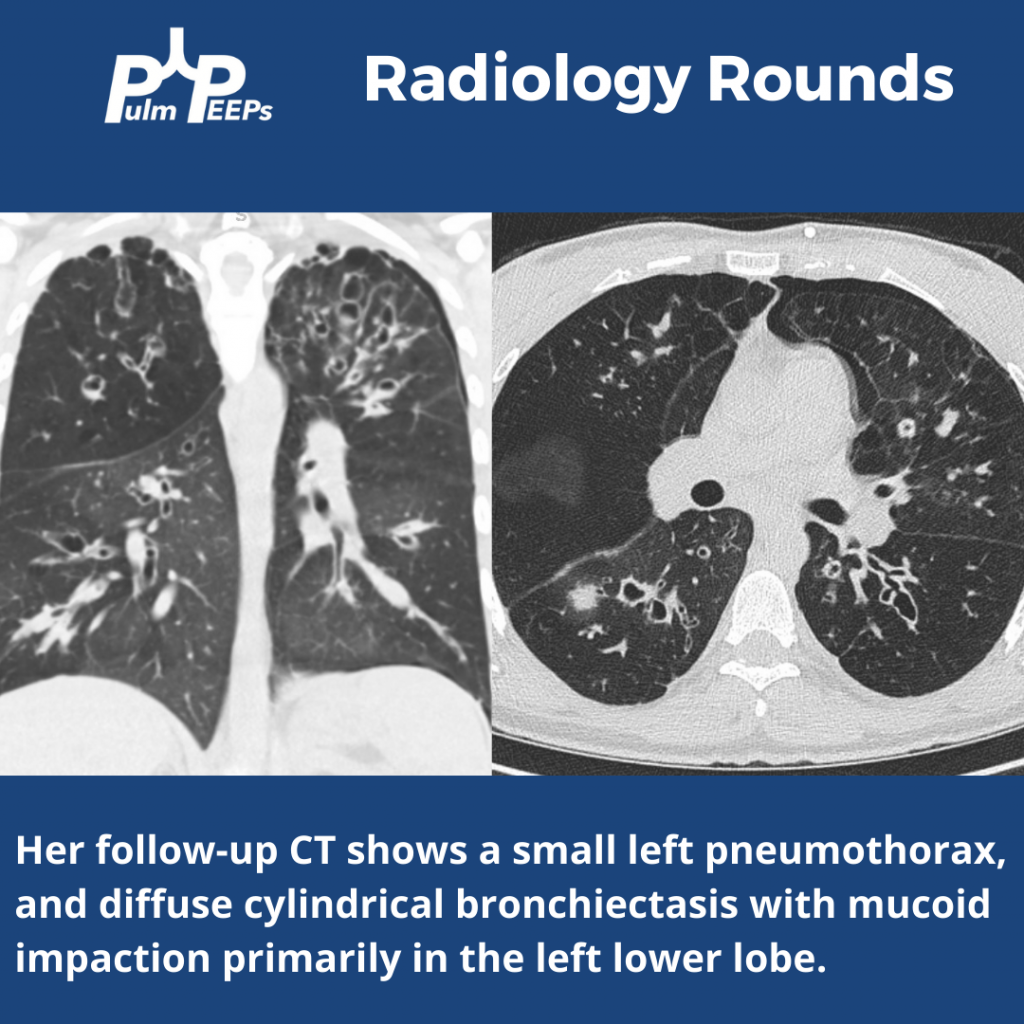
We are excited to bring you another #RadiologyRounds which applies some of the knowledge from our most recent episode on pneumothorax.
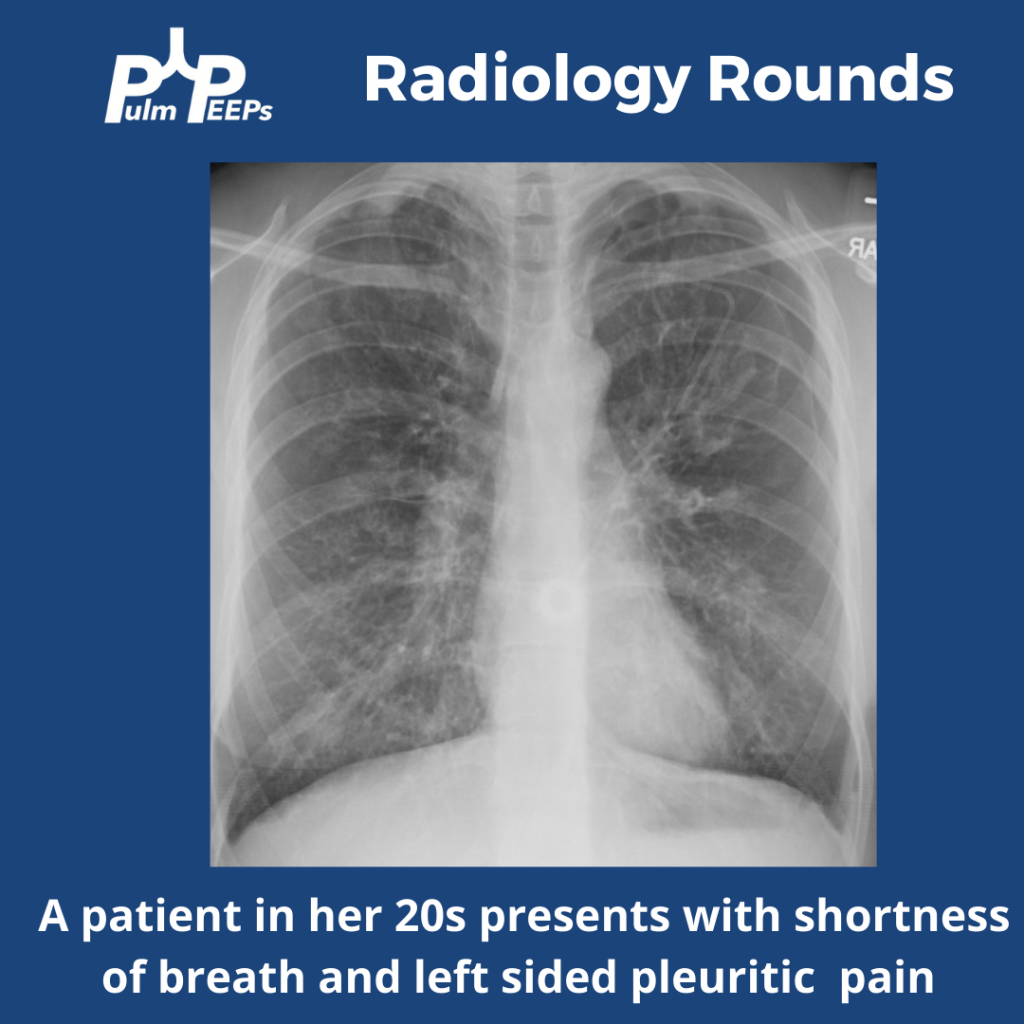
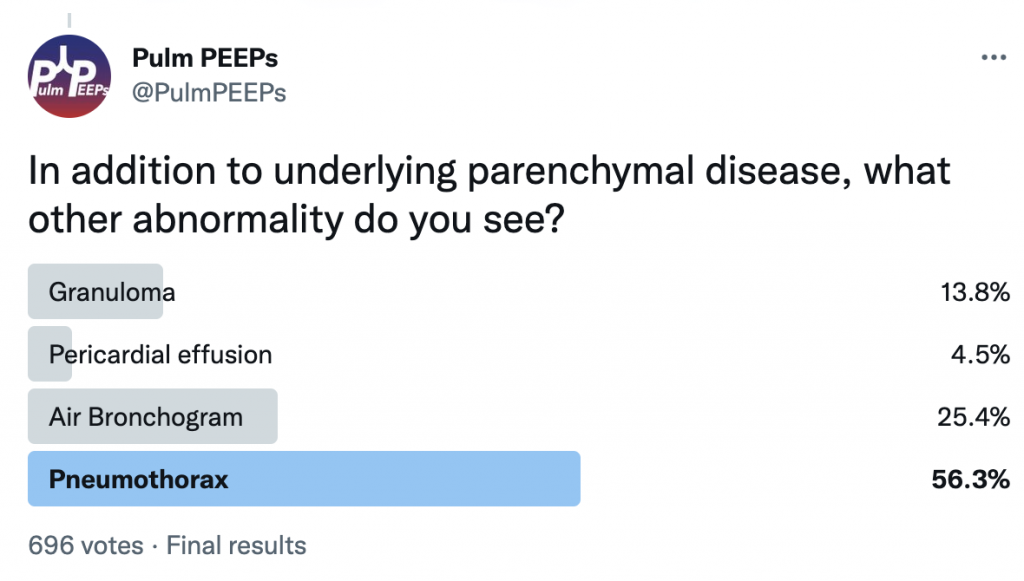
She is presenting with a 1.5 cm left pneumothorax. You can see lucency representing air in the pleural space. There are a lack of blood vessels or lung markings extending to the periphery and you can see the visceral pleura.
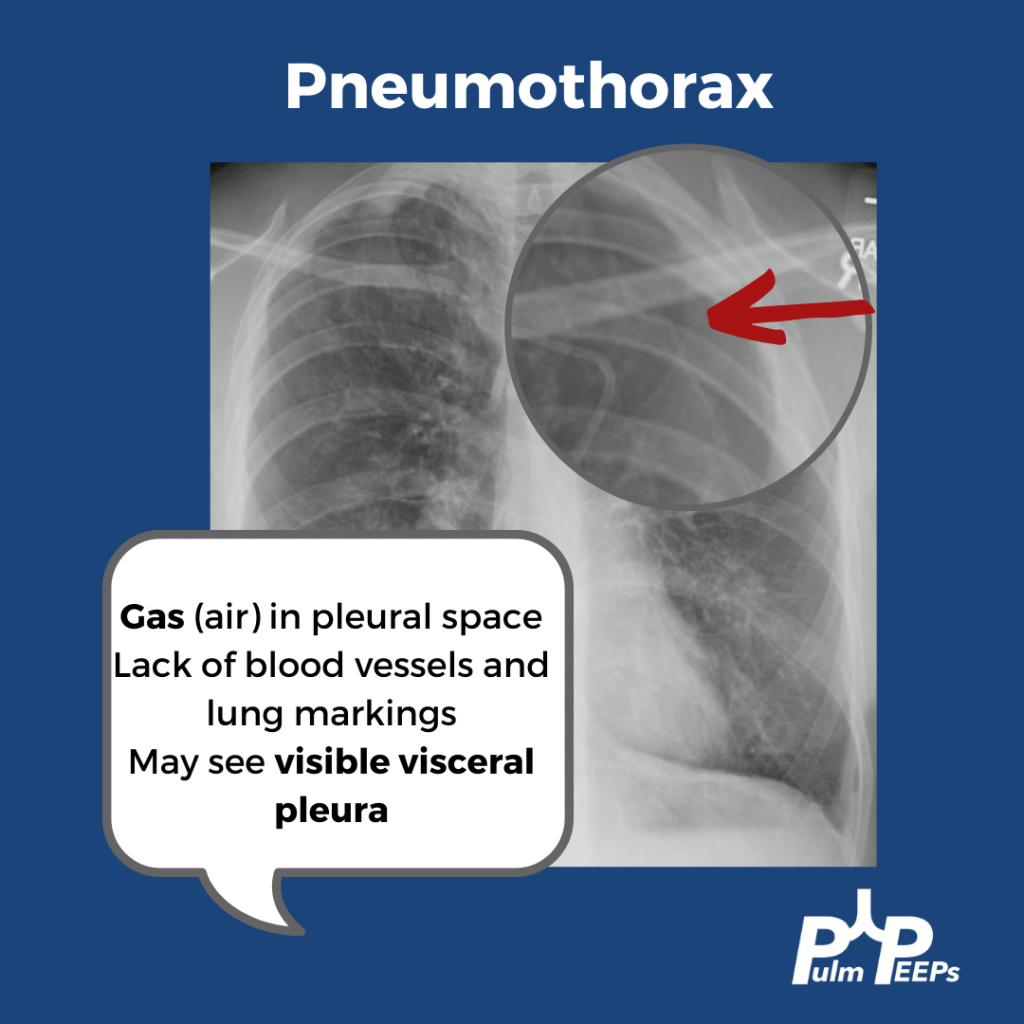
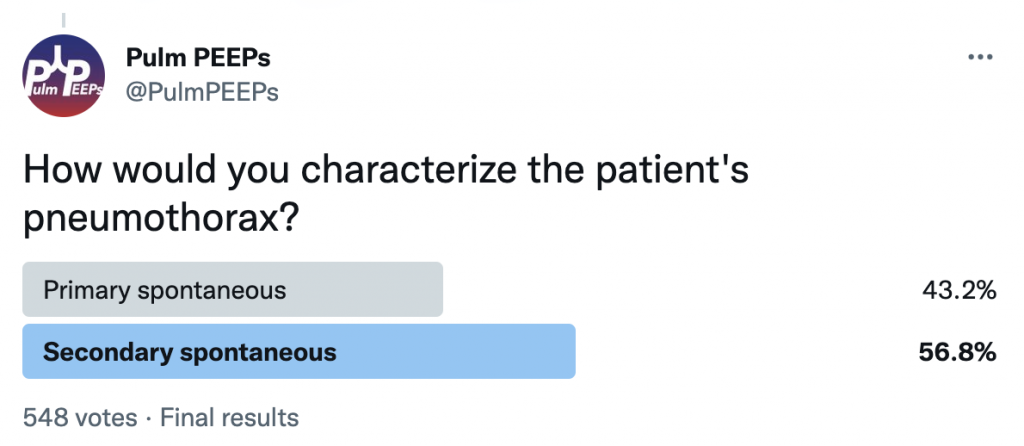
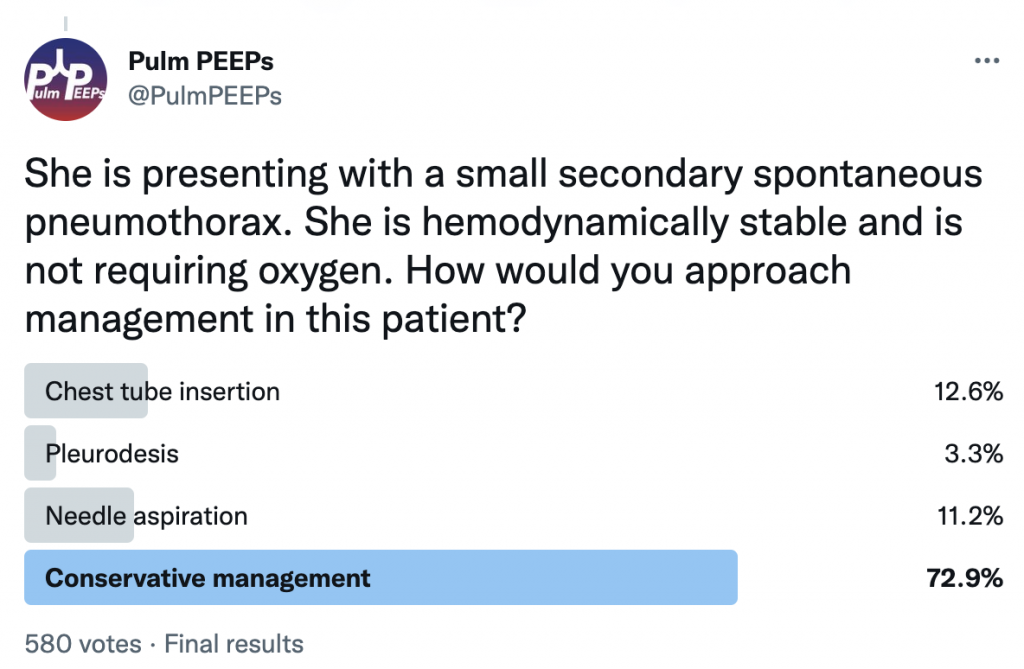
She is presenting with her first pneumothorax which is a small, spontaneous pneumothorax secondary to her underlying cystic lung disease. She was managed conservatively and followed closely outpatient with ultimate resolution of her pneumothorax.
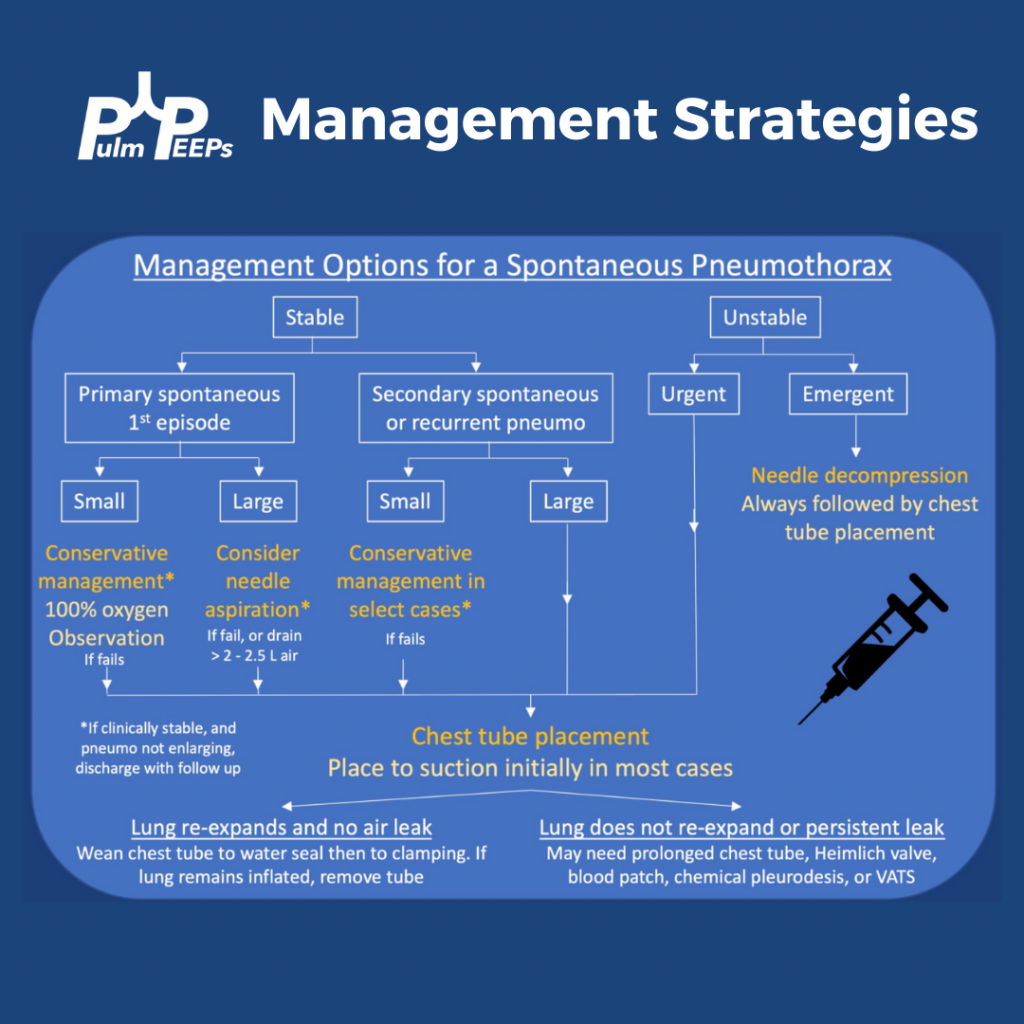
This week on Pulm PEEPs we are resuming our Top Consults series with a common pulmonary presentation that can range from incidental to life-threatening: pneumothorax. We will talk through three different cases and review assessments and common management strategies. Make sure to subscribe to our show wherever you listen to podcasts, rate and review us, and visit our website to catch up on all our old content.
Meet Our Guests
Christine Argento is an Associate Professor of Medicine at Johns Hopkins Hospital and specializes in Interventional Pulmonology.
Charlie Murphy received his medical degree from LSU School of Medicine in New Orleans and completed his internal medicine residency at the Montefiore-Einstein Internal Medicine Residency Program. He is currently a Pulmonary and Critical Care fellow at New York-Presbyterian Hospital / Columbia University Medical Center, where he is one of the chief fellows.
Consult Patients
Barry is a 26-year-old man who came to the emergency department with acute onset of shortness of breath. He is tachypneic to 26, saturating 88% on RA so he was put on NC and is now 95% at 4L, HR 120, BP 145/85. There is only limited history but he reports he has never had anything like this before. His CXR shows a pneumothorax 5cm from the apex.
Larry is a 22-year-old man with normal HR and BP, saturating 96% on RA and breathing 14 x a minute. He has a CXR that shows a small pneumothorax. He has no past medical history and has never had a pneumothorax before, but he is a 1 PPD smoker and smokes marijuana.
Carrie is a 54-year-old woman who has been admitted with a COPD exacerbation. She has a history of emphysema, is not on home oxygen, and came in 2 days ago with worsening dyspnea and increased productive cough. She has been being treated with nebulizers every 4 hours, azithromycin, steroids, and supplemental O2 at 2L NC/ minute and never required NIPPV. This morning she had a coughing spell and significant chest pain and a CXR shows a moderate-sized left-sided pneumothorax. She is on 10L NC now with tachypnea to 26, and HR 105 but stable blood pressure.
Key Learning Points
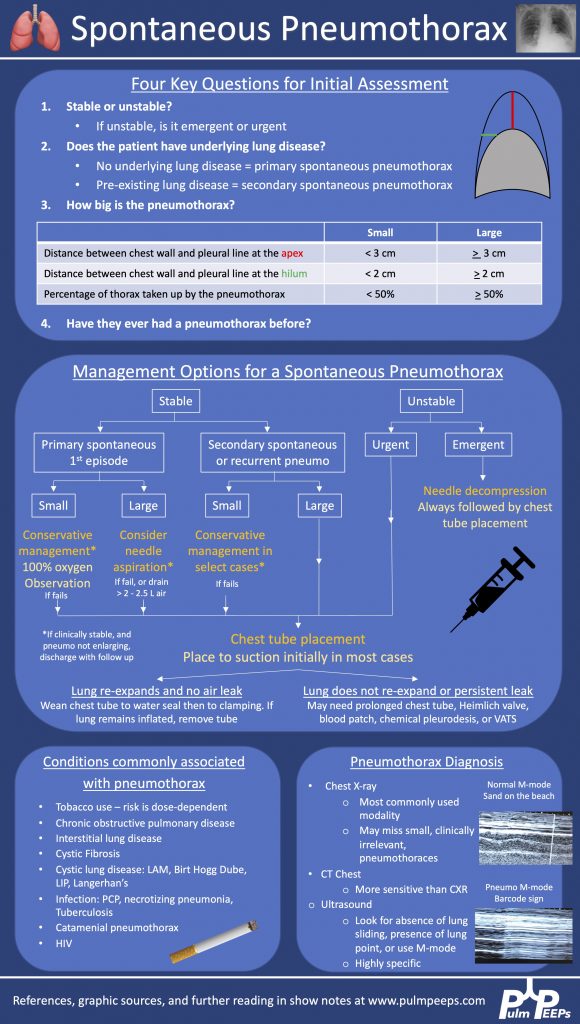
Management options for a persistent air leak
— Conservative management: continue chest tube to suction
— Heimlich valve – can discharge a patient with this valve if they are stable to water seal, but don’t tolerate clamping
— Blood patch – inject the patient’s own blood into the chest tube to try to heal any pleural defect
— Chemical pleurodesis – inject talc powder, doxycycline, or another substance through the chest tube to cause pleural irritation and closure of the pleural space
— Endobronchial valve – off-label use
— VATS – surgical pleurodesis, resection of blebs
References and links for further reading
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More