Today, we continue our review of the Global Initiative for Asthma (GINA) guidelines on asthma. We’ve covered asthma diagnosis and phenotyping, and the initial approach to therapy. On today’s episode we’re talking about biologic therapies for asthma and will cover everything from when to consider starting them, which to choose, and what to monitor for after a patient is started. To help us with this exciting topic we’re joined by an expert in the field. We again have a great infographic prepared along with the episode, and a boards-style question for your review.
Meet Our Guest
Megan Conroy is an Assistant Professor of Medicine at The Ohio State University, and is also the associate program director for curriculum and quality in the Pulmonary and Critical Care Medicine Fellowship. Megan’s clinical area of expertise involves asthma and biologic therapies and she was recently recognized for her work in this area as the 2024 CHEST Airway Disorders Network Rising Star Award.
Meet Our Co-Hosts
Rupali Sood grew up in Las Vegas, Nevada and made her way over to Baltimore for medical school at Johns Hopkins. She then completed her internal medicine residency training at Massachusetts General Hospital before returning back to Johns Hopkins, where she is currently a second year pulmonary and critical care medicine fellow alongside Tom. Rupali’s interests include interstitial lung disease, particularly as related to oncologic drugs. And she also loves bedside medical education.
Tom Di Vitantonio is originally from New Jersey and attended medical school at Rutgers, New Jersey Medical School in Newark. He then completed his internal medicine residency at Weill Cornell, where he also served as a chief resident. He currently is a second year pulmonary and critical care medicine fellow at Johns Hopkins, and he’s passionate about caring for critically ill patients, how we approach the management of pulmonary embolism, and also about medical education of trainees to help them be more confident and patient centered in the care they have going forward.
Key Learning Points
Core Themes and Clinical Relevance
- ~20% of asthma patients have difficult-to-control asthma.
- Only ~5% have severe asthma after optimizing inhaler use, addressing comorbidities, and ensuring adherence.
- Elevated eosinophils (≥150/µL)
- High IgE
- High fractional exhaled nitric oxide (FeNO)
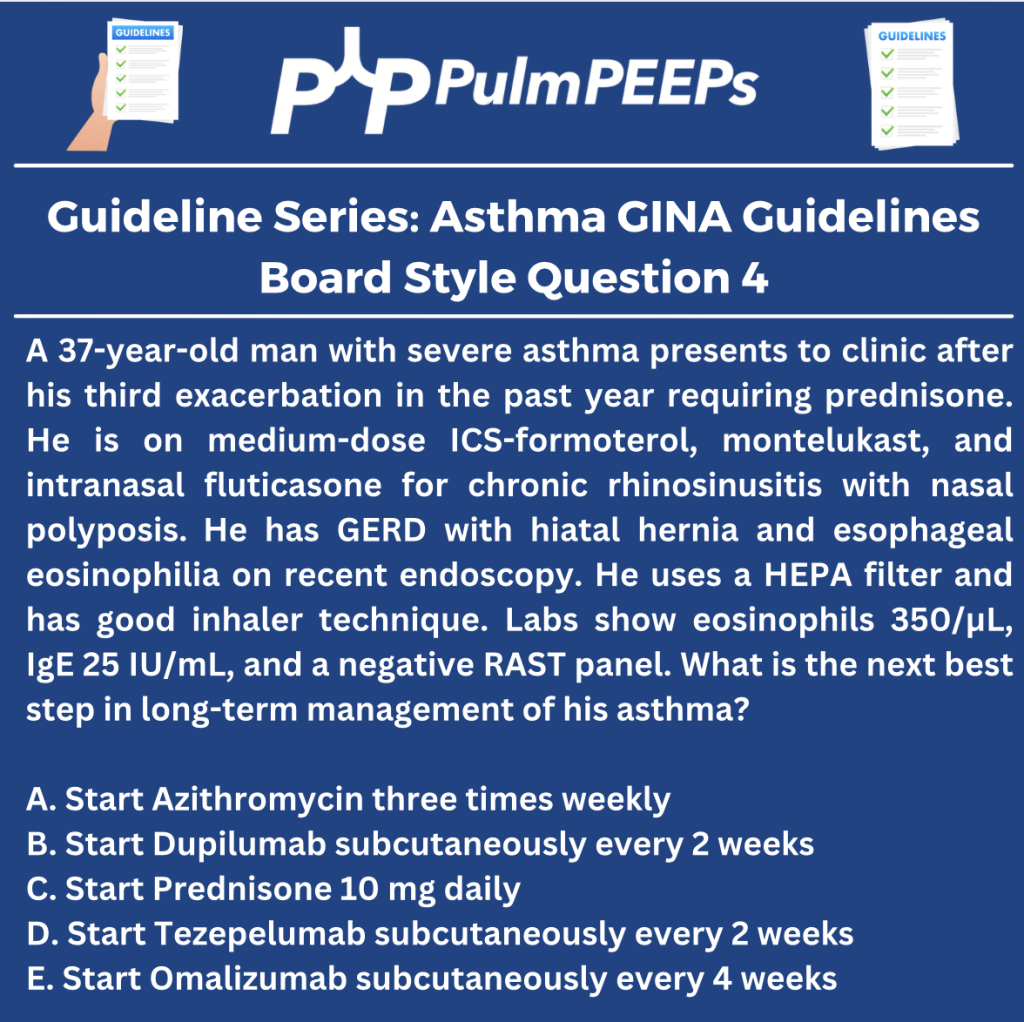
Choosing the Right Biologic
- Nasal polyps, EoE, atopic dermatitis → Dupilumab
- Strong allergic sensitization → Omalizumab
- T2-low or mixed features → Tezepelumab
Monitoring and Follow-Up
- Look for ≥50% reduction in exacerbations or steroid use
- Check spirometry, asthma control, and side effects
- Dupilumab → monitor eosinophils (risk of HES)
- Omalizumab → ensure access to epinephrine auto-injector
- Limited data, but omalizumab has most evidence supporting safety.
- Expert consensus supports continuing or initiating biologics if benefits outweigh risks.
- Only Tezepelumab is indicated.
Clinical Pearls
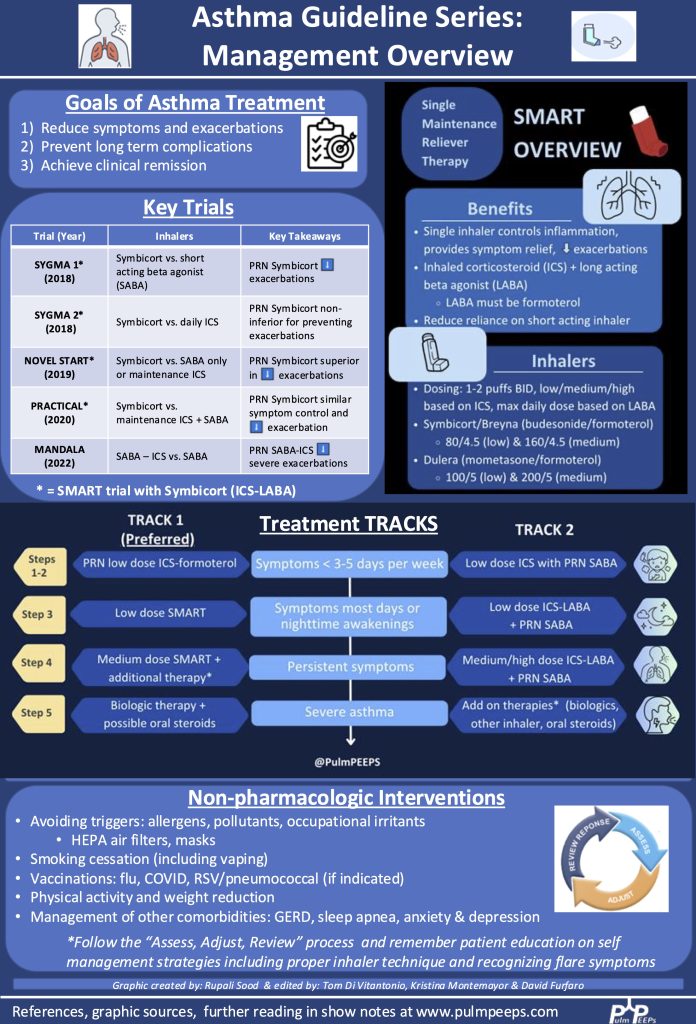
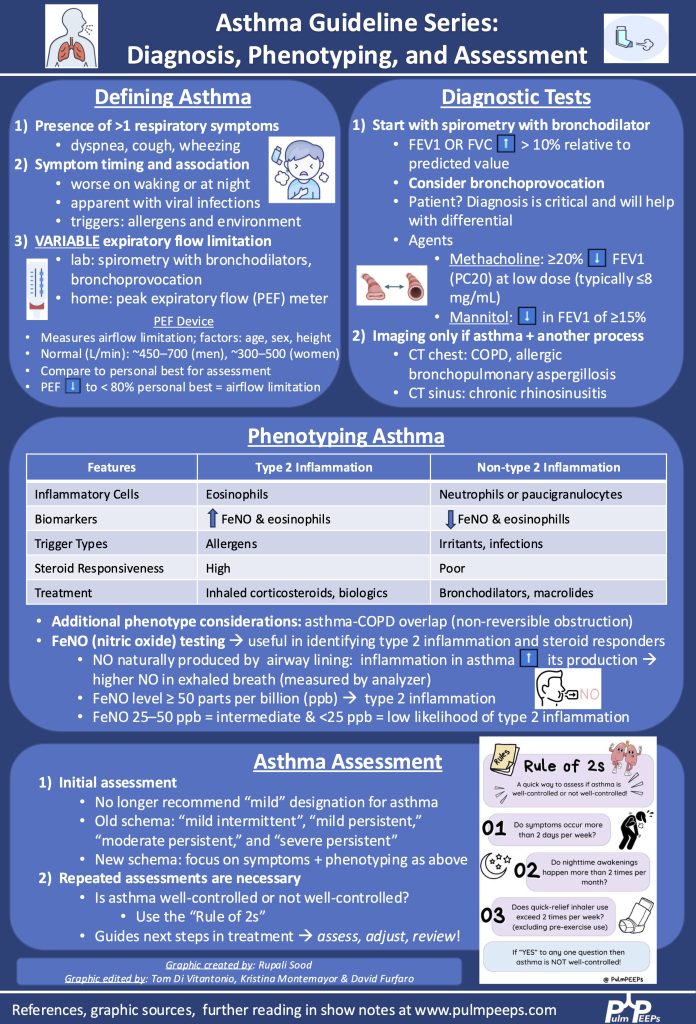
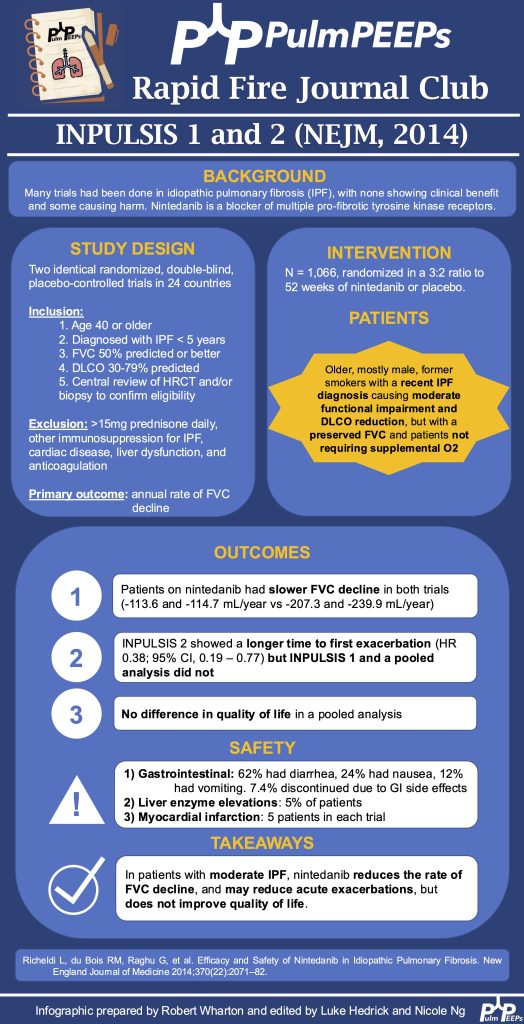
Infographic

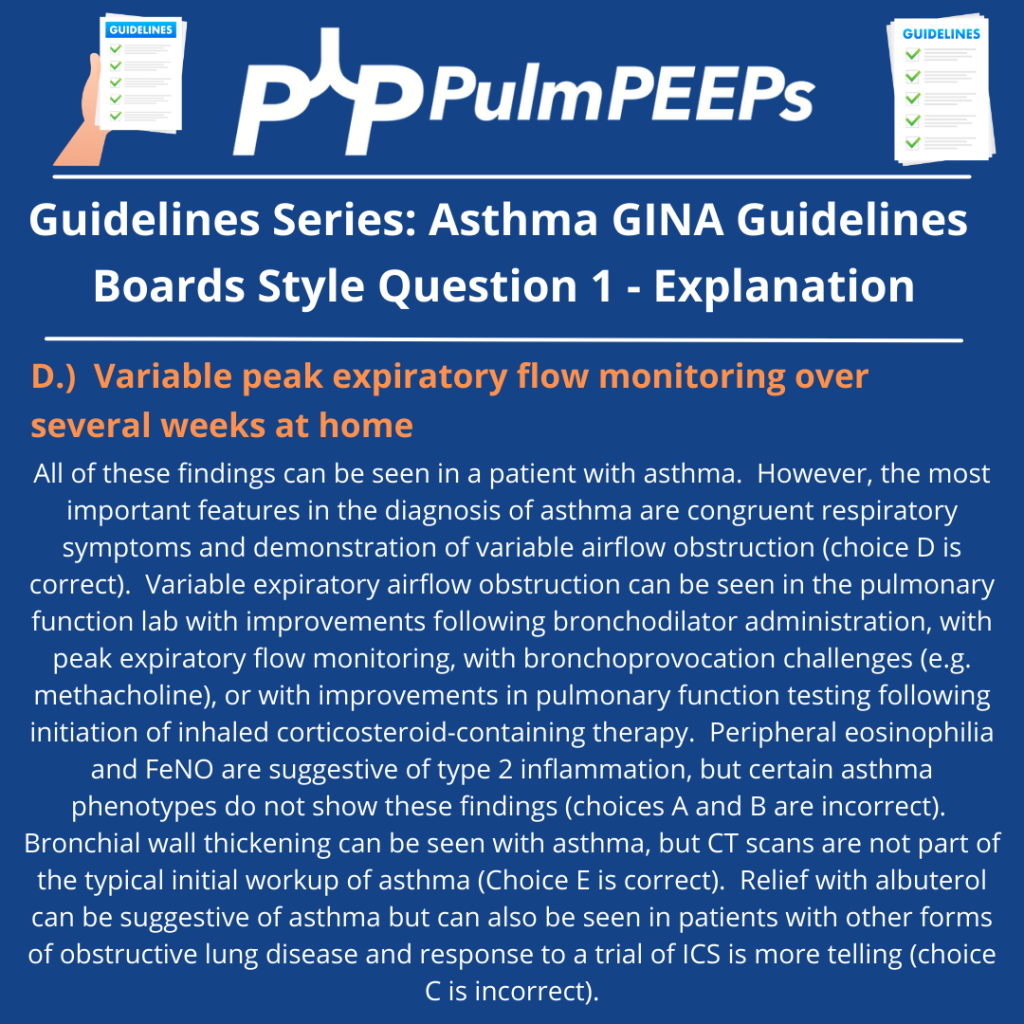
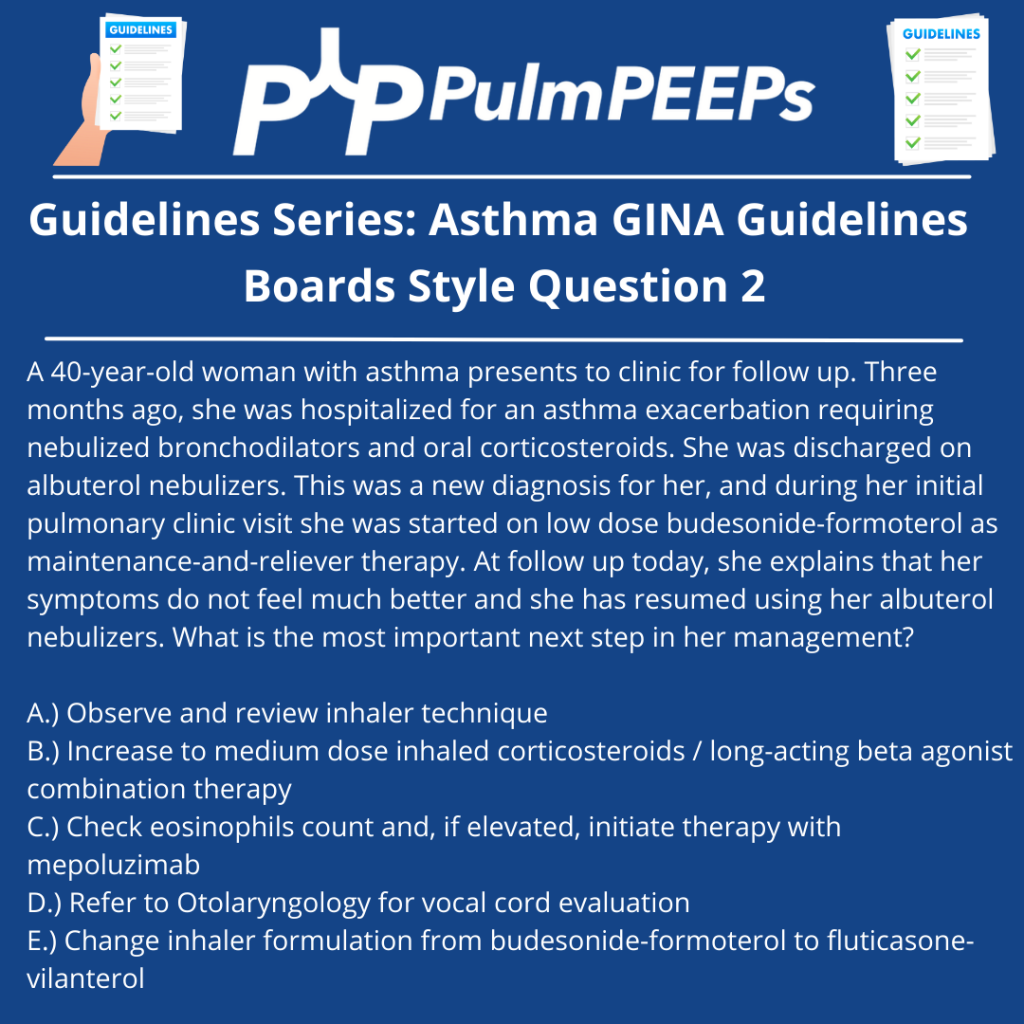
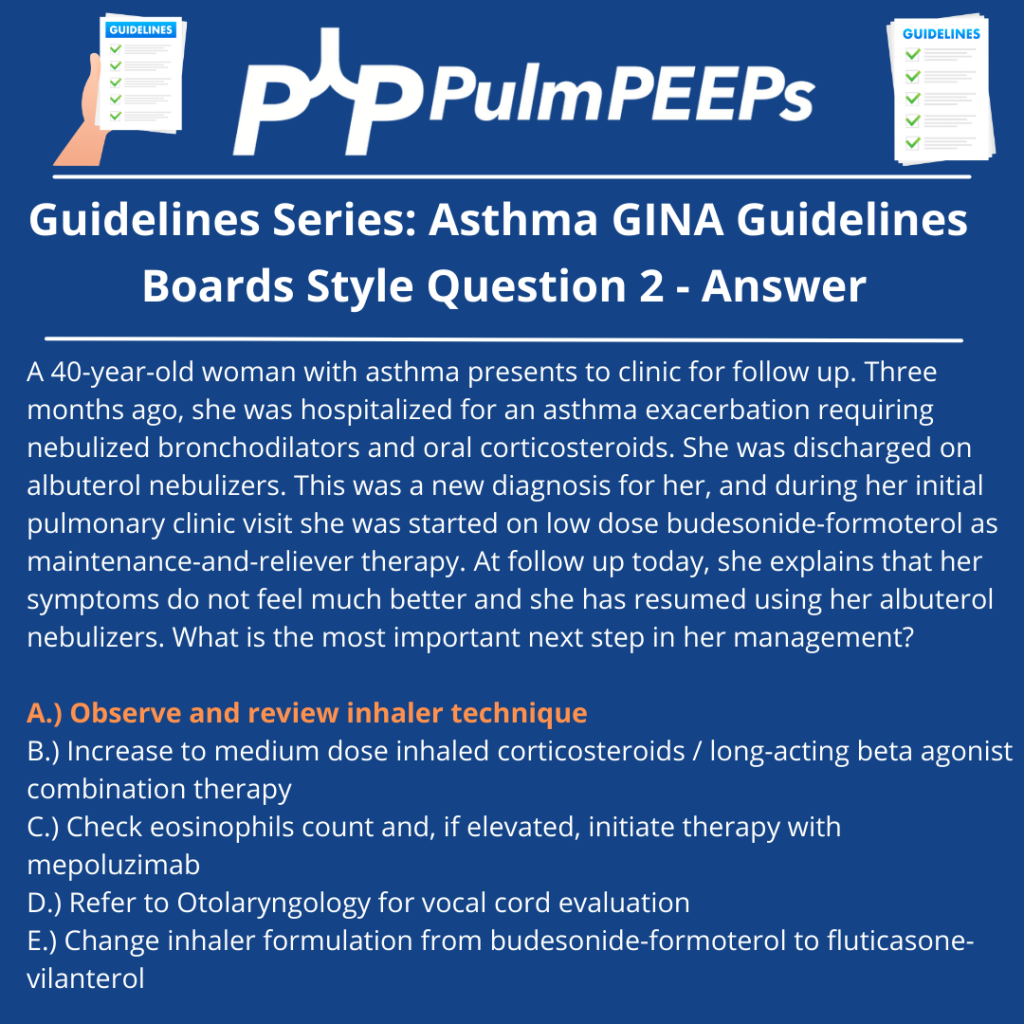
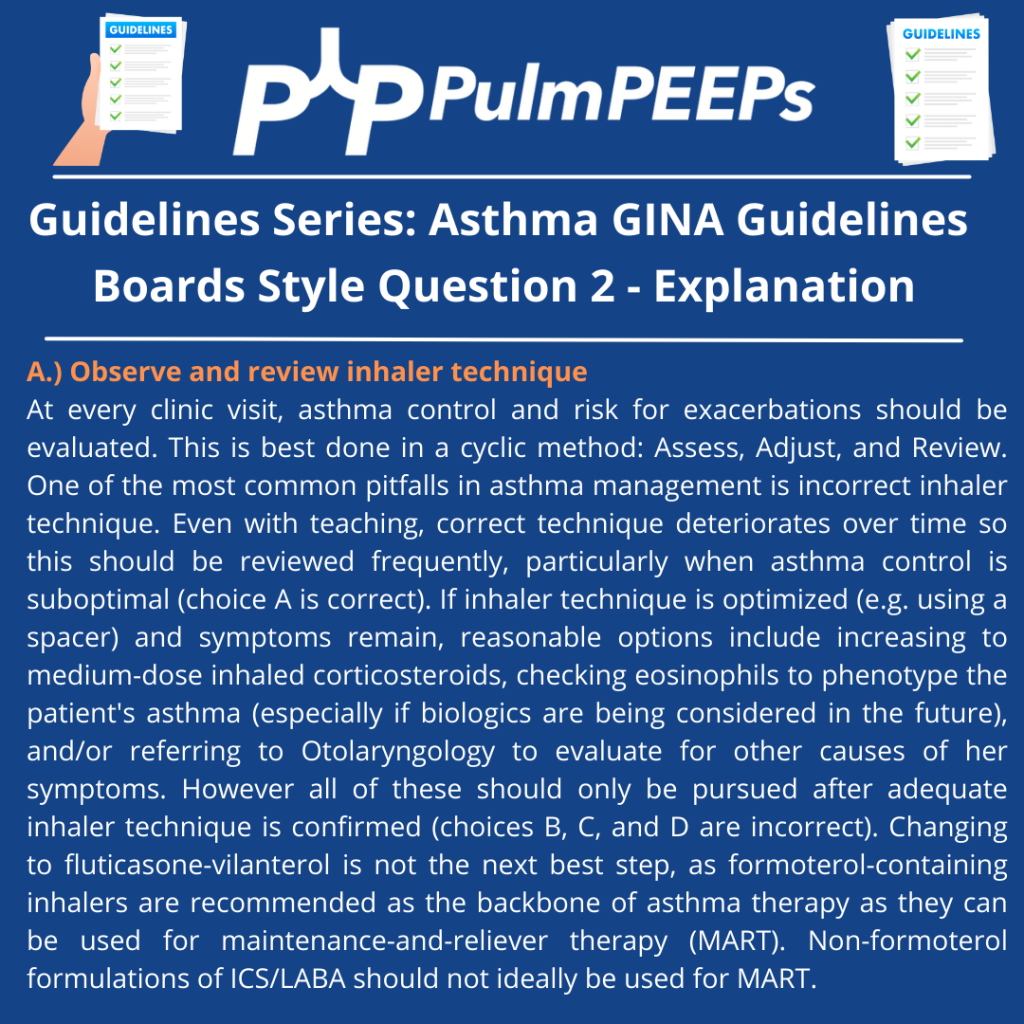
Boards Style Question
References:
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More