This week on Pulm PEEPs, we are continuing our Top Consults series with a discussion on the work-up and diagnosis of Pulmonary Hypertension. See our prior Radiology Rounds on signs of PAH on CT scan, and listen to our follow-up episode on right heart catheterizations for some background before this episode… or dive right in! We’ll cover everything from history and physical, to recent guideline changes in the definition of PH, and much, much more!
Meet Our Guests
Erika Berman Rosenzweig is a Professor of Pediatrics and the Director of the Pulmonary Hypertension Center and CTEPH Program at Columbia University Medical Center / New-York Presbyterian Hospital. She is an active member of the Pulmonary Hypertension Association, was the Editor-in-Chief of Advances in Pulmonary Hypertension and is on the Scientific Board of the World Symposium on PH.
Catherine Simpson is an Assistant Professor of Medicine at Johns Hopkins Hospital and is one of the faculty members in our Pulmonary Hypertension group. Her clinical and research areas of expertise are in pulmonary vascular disease and right heart function. Her research is focused on novel biomarker discovery and metabolomics in pulmonary vascular disease.
Cyrus Kholdani is an Instructor in Medicine at Beth Israel Deaconess Medical Center and Harvard Medical School. He is also the director of the Pulmonary Hypertension Program at BIDMC, and is actively involved in clinical care and clinical research in a variety of pulmonary vascular disease domains.
Consult Patient
Ms. Pamela Harris (PH) is a 47-year-old woman with PMH of migraines, obesity s/p gastric sleeve (BMI now 33), and a history of remote DVT in her 20s while on OCP s/p 6 months of AC who is referred to pulmonary hypertension clinic for evaluation of dyspnea on exertion. She has actually had dyspnea for some time and previously it has been attributed to her weight. Based on this, she pursued a gastric sleeve and has lost 55 pounds, but continues to have shortness of breath. She has no cough, and does not get dyspnea at rest, but notes that after 1 flight of stairs, or 2-3 blocks on flat ground she has shortness of breath. She saw her PCP and had basic labs, basic spirometry, and an echocardiogram. He did not note anything significant on examination in the notes.
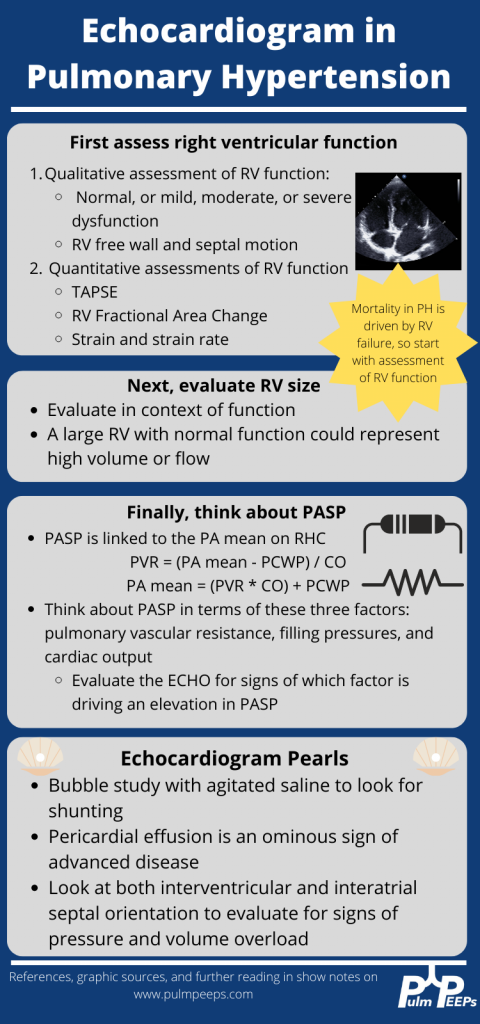
The labs had no anemia, and normal renal and liver function. Her serum bicarbonate was 25 and there was no blood gas. Spirometry showed an FVC 82% predicted, FEV1 83% predicted, and FEV1/FVC was 99% predicted. The echocardiogram had normal LVEF, mild LVH, normal RV size and function qualitatively. There was mild TR with tricuspid valve peak regurgitant velocity of 3.4 m/sec. The estimated PASP + RA pressure (based on normal IVC diameter 2.1 cm) was 46 mmHg.
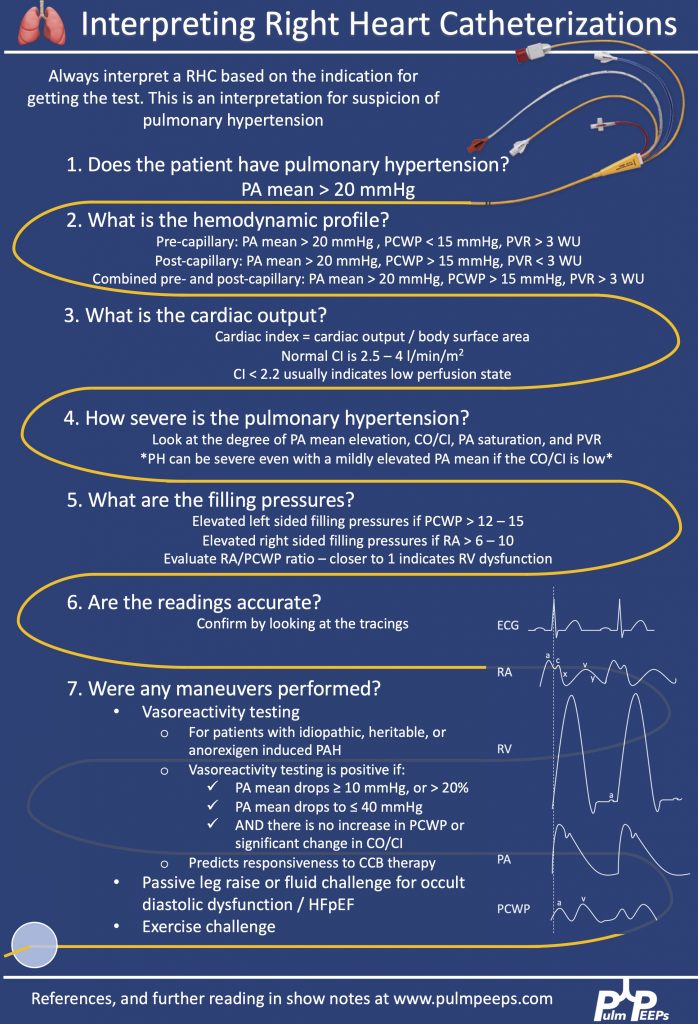
RHC: Systemic BPs 140s/90s, with O2 saturations 97-98% on RA throughout. RA mean pressure was 9, RV was 48 with an RVEDP of 17, PA was 48/27 with mean of 34, and PCWP mean was 11. CO/CI by Fick was 5.56 / 2.42, and by thermo was similar, 5.8 / 2.52. Her PA sat was 62%, and PVR was 3.97 WU.
Key Learning Points
History
- Understand the constellation of symptoms and the functional limitation
- The goal is to assign a WHO functional class by the end of the visit
- Evaluate the time course and evolution of the symptoms
- Concerning symptoms that need to be addressed
- Palpitations
- Pre-syncope
- Syncope
- Chest pain
- LE edema
- Evaluate for risk factors to explain or contribute to pulmonary hypertension
- Signs or symptoms of OSA
- Signs or symptoms of auto-immune disease
- Raynauds
- Skin changes
- Family history
- Heritable lung disease
- Clotting disorders
- Auto-immune disease
- Social history
- Exposure history
- Smoking
Physical Exam
- Look for signs that confirm PH
- Loud P2
- Accentuated with elevated PVR
- Can hear pretty early on. Could be one of the earliest findings
- TR murmur – pansystolic murmur at RUSB
- Diastolic murmur if severe pulmonary insufficiency
- Loud P2
- Look for signs of right heart failure
- JVD
- S4 gallop – later in course
- RV heave – later in course
- Peripheral edema
- Pulsatile liver or hepatosplenomegaly
- Look for signs of other secondary causes of PH
- Mitral regurgitation or aortic stenosis murmur
- Asymmetric lower extremity edema
- Pulmonary edema
- Skin findings concerning for auto-immune disease or liver disease
- Arthritis
Work up for etiology of PH
- CBC with diff – myeloproliferative and hemolytic anemia
- CMP – renal function, liver function
- Serologies – lupus, scleroderma, vasculitis – broad evaluation
- HIV, hepatitis
- Liver duplex if concerned
- ECHO with bubble
- Consider cardiac MRI
- History of toxin and anorexigenic use
- CT scan of the chest
- PFTs including lung volumes and DLCO to evaluate for lung disease
- Pulse oximetry at rest and with exercise
- A sleep study or nocturnal oximetry
- V/Q scan for all patients
References and links for further reading
- Bonno EL, Viray MC, Jackson GR, Houston BA, Tedford RJ. Modern Right Heart Catheterization: Beyond Simple Hemodynamics. Advances in Pulmonary Hypertension. 2020;19(1):6-15. doi:10.21693/1933-088X-19.1.6
- Augustine DX, Coates-Bradshaw LD, Willis J, et al. Echocardiographic assessment of pulmonary hypertension: a guideline protocol from the British Society of Echocardiography. Echo Res Pract. 2018;5(3):G11-G24. doi:10.1530/ERP-17-0071
- Callan P, Clark AL. Right heart catheterisation: indications and interpretation. Heart. 2016;102(2):147-157. doi:10.1136/heartjnl-2015-307786
- Chokkalingam Mani B, Chaudhari SS. Right Heart Cardiac Catheterization. In: StatPearls. StatPearls Publishing; 2022. Accessed April 18, 2022. http://www.ncbi.nlm.nih.gov/books/NBK557404/
- D’Alto M, Dimopoulos K, Coghlan JG, Kovacs G, Rosenkranz S, Naeije R. Right Heart Catheterization for the Diagnosis of Pulmonary Hypertension: Controversies and Practical Issues. Heart Failure Clinics. 2018;14(3):467-477. doi:10.1016/j.hfc.2018.03.011
- Galiè N, McLaughlin VV, Rubin LJ, Simonneau G. An overview of the 6th World Symposium on Pulmonary Hypertension. European Respiratory Journal. 2019;53(1). doi:10.1183/13993003.02148-2018
- Rosenkranz S, Preston IR. Right heart catheterisation: best practice and pitfalls in pulmonary hypertension. European Respiratory Review. 2015;24(138):642-652. doi:10.1183/16000617.0062-2015
Podcast: Play in new window | Download
Subscribe: Apple Podcasts | Spotify | Amazon Music | Android | iHeartRadio | Podcast Index | RSS | More
